Back
Oral Paper Presentation
Annual Scientific Meeting
Session: Presidential Plenary Session 2
6 - Endoscopic vs Conservative Treatment for Bleeding Peptic Ulcer With Adherent Clot: A Comprehensive Systematic Review and Meta-Analysis of Randomized Controlled Trials
Monday, October 24, 2022
9:30 AM – 9:42 AM ET
Location: Hall C2
.jpg)
Azizullah Beran, MD
University of Toledo
Toledo, OH
Presenting Author(s)
Azizullah Beran, MD1, Yasir Al-Abboodi, MD1, Sami Ghazaleh, MD1, Wasef Sayeh, MD1, Mouhand F. Mohamed, MD, MSc2, Khaled Elfert, MD, MRCP3, Rami Musallam, MD4, Anas Alsughayer, MD5, David Farrow, MD1, Syed Hamaad Rahman, DO6, Mohammad Al-Haddad, MD, MSc7
1University of Toledo, Toledo, OH; 2Warren Alpert Medical School of Brown University, Providence, RI; 3SBH Health System, New York, NY; 4St. Vincent Charity Medical Center, Cleveland, OH; 5University of Toledo Medical Center, Toledo, OH; 6Methodist Dallas Medical Center, Dallas, TX; 7Indiana University School of Medicine, Indianapolis, IN
Introduction: Peptic ulcer disease (PUD) is the leading cause of upper GI bleeding. PUDs with an adherent clot (Forrest IIb) are associated with a high risk of rebleeding and mortality. However, the optimal management of bleeding PUD with adherent clots, including endoscopic or conservative therapy, remains unclear. The most recent ACG guidelines in 2021 did not clearly endorse endoscopic treatment for bleeding PUDs with adherent clot as opposed to medical therapy. We performed this systematic review and meta-analysis to compare the endoscopic and conservative therapeutic approaches to managing bleeding PUDs with adherent clot.
Methods: We systematically searched MEDLINE, EMBASE, and the Web of Science databases through May 15, 2022, to include all randomized controlled trials (RCTs) comparing the endoscopic and conservative therapeutic approaches for bleeding PUDs with adherent clots. The outcomes of interest in our meta-analysis were rebleeding, need for surgery, and mortality. The random-effects model was used to calculate the weighted pooled risk ratio (RR) with the corresponding 95% confidence intervals (CI) of our desired outcome. A P-value < 0.05 was considered statistically significant. Heterogeneity was assessed using the Higgins I2 index (I2 values >50% implied the presence of significant heterogeneity).
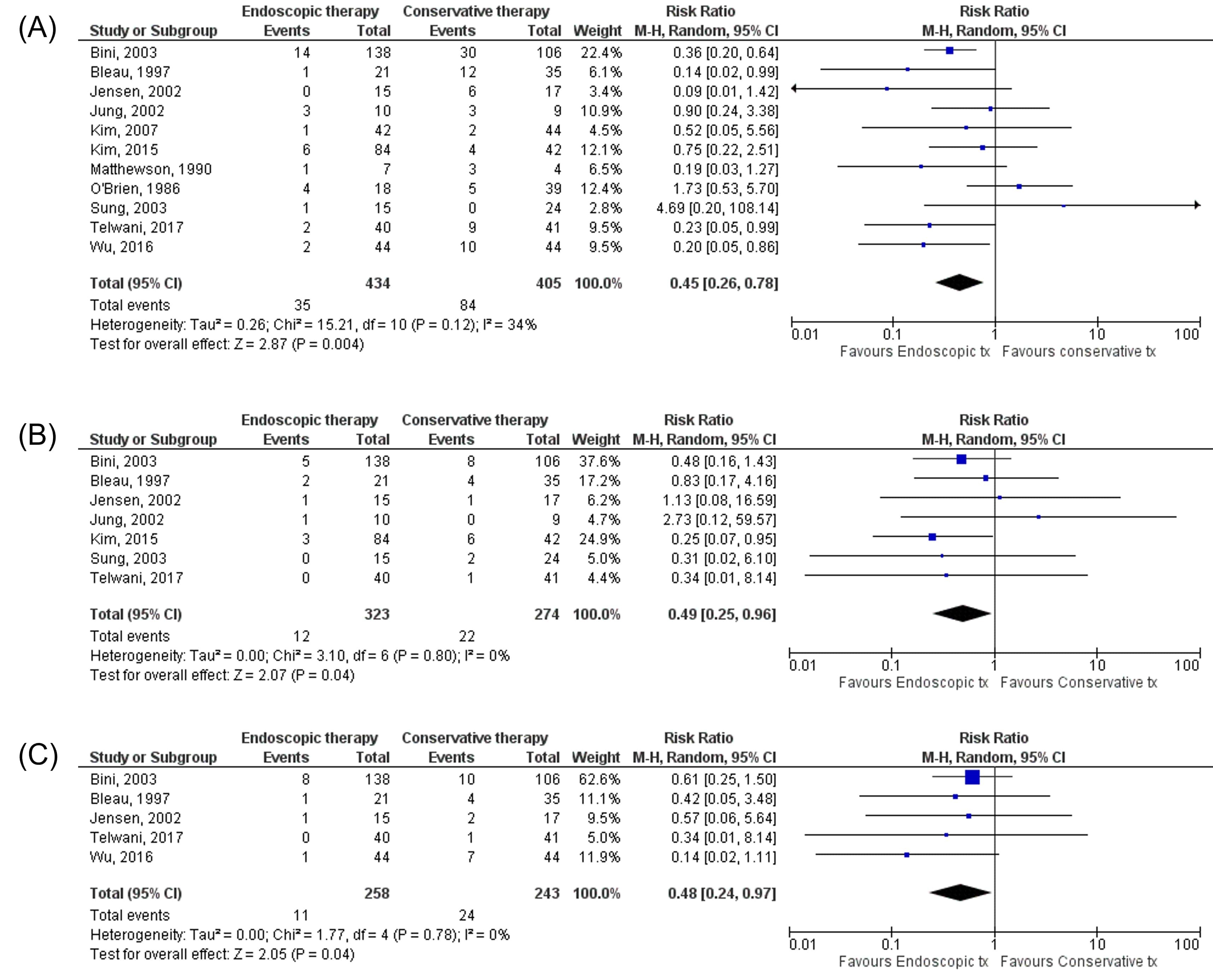
Results: Eleven RCTs with 839 patients (434 received endoscopic therapy vs. 405 received conservative therapy) were included. Endoscopic therapy group underwent clot removal and treatment of the underlying lesion with thermocoagulation, electrocoagulation, injection of sclerosants such as epinephrine or ethanol, or hemoclipping. Rebleeding occurred in 8.1% of patients in the endoscopic therapy group, compared to 20.7% in the conservative therapy group (RR 0.45, 95% CI 0.26-0.78, P=0.004, I2=34%, Figure 1A). We observed lower mortality of 3.7% in the endoscopic therapy group compared to 8% in the conservative therapy group (RR 0.49, 95% CI 0.25-0.96, P=0.04, I2=0%, Figure 1B). In addition, the need for surgery was significantly lower in the endoscopic therapy group (4.3%) compared to the conservative therapy group (9.9%) (RR 0.48, 95% CI 0.24-0.97, P=0.04, I2=0%, Figure 1C).
Discussion: Our meta-analysis demonstrated that endoscopic therapy is superior to conservative treatment for bleeding PUDs with an adherent clot regarding rebleeding, need for surgery, and mortality. However, large-scale RCTs are needed to validate our findings.
Disclosures:
Azizullah Beran, MD1, Yasir Al-Abboodi, MD1, Sami Ghazaleh, MD1, Wasef Sayeh, MD1, Mouhand F. Mohamed, MD, MSc2, Khaled Elfert, MD, MRCP3, Rami Musallam, MD4, Anas Alsughayer, MD5, David Farrow, MD1, Syed Hamaad Rahman, DO6, Mohammad Al-Haddad, MD, MSc7, 6, Endoscopic vs Conservative Treatment for Bleeding Peptic Ulcer With Adherent Clot: A Comprehensive Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Toledo, Toledo, OH; 2Warren Alpert Medical School of Brown University, Providence, RI; 3SBH Health System, New York, NY; 4St. Vincent Charity Medical Center, Cleveland, OH; 5University of Toledo Medical Center, Toledo, OH; 6Methodist Dallas Medical Center, Dallas, TX; 7Indiana University School of Medicine, Indianapolis, IN
Introduction: Peptic ulcer disease (PUD) is the leading cause of upper GI bleeding. PUDs with an adherent clot (Forrest IIb) are associated with a high risk of rebleeding and mortality. However, the optimal management of bleeding PUD with adherent clots, including endoscopic or conservative therapy, remains unclear. The most recent ACG guidelines in 2021 did not clearly endorse endoscopic treatment for bleeding PUDs with adherent clot as opposed to medical therapy. We performed this systematic review and meta-analysis to compare the endoscopic and conservative therapeutic approaches to managing bleeding PUDs with adherent clot.
Methods: We systematically searched MEDLINE, EMBASE, and the Web of Science databases through May 15, 2022, to include all randomized controlled trials (RCTs) comparing the endoscopic and conservative therapeutic approaches for bleeding PUDs with adherent clots. The outcomes of interest in our meta-analysis were rebleeding, need for surgery, and mortality. The random-effects model was used to calculate the weighted pooled risk ratio (RR) with the corresponding 95% confidence intervals (CI) of our desired outcome. A P-value < 0.05 was considered statistically significant. Heterogeneity was assessed using the Higgins I2 index (I2 values >50% implied the presence of significant heterogeneity).
Results: Eleven RCTs with 839 patients (434 received endoscopic therapy vs. 405 received conservative therapy) were included. Endoscopic therapy group underwent clot removal and treatment of the underlying lesion with thermocoagulation, electrocoagulation, injection of sclerosants such as epinephrine or ethanol, or hemoclipping. Rebleeding occurred in 8.1% of patients in the endoscopic therapy group, compared to 20.7% in the conservative therapy group (RR 0.45, 95% CI 0.26-0.78, P=0.004, I2=34%, Figure 1A). We observed lower mortality of 3.7% in the endoscopic therapy group compared to 8% in the conservative therapy group (RR 0.49, 95% CI 0.25-0.96, P=0.04, I2=0%, Figure 1B). In addition, the need for surgery was significantly lower in the endoscopic therapy group (4.3%) compared to the conservative therapy group (9.9%) (RR 0.48, 95% CI 0.24-0.97, P=0.04, I2=0%, Figure 1C).
Discussion: Our meta-analysis demonstrated that endoscopic therapy is superior to conservative treatment for bleeding PUDs with an adherent clot regarding rebleeding, need for surgery, and mortality. However, large-scale RCTs are needed to validate our findings.
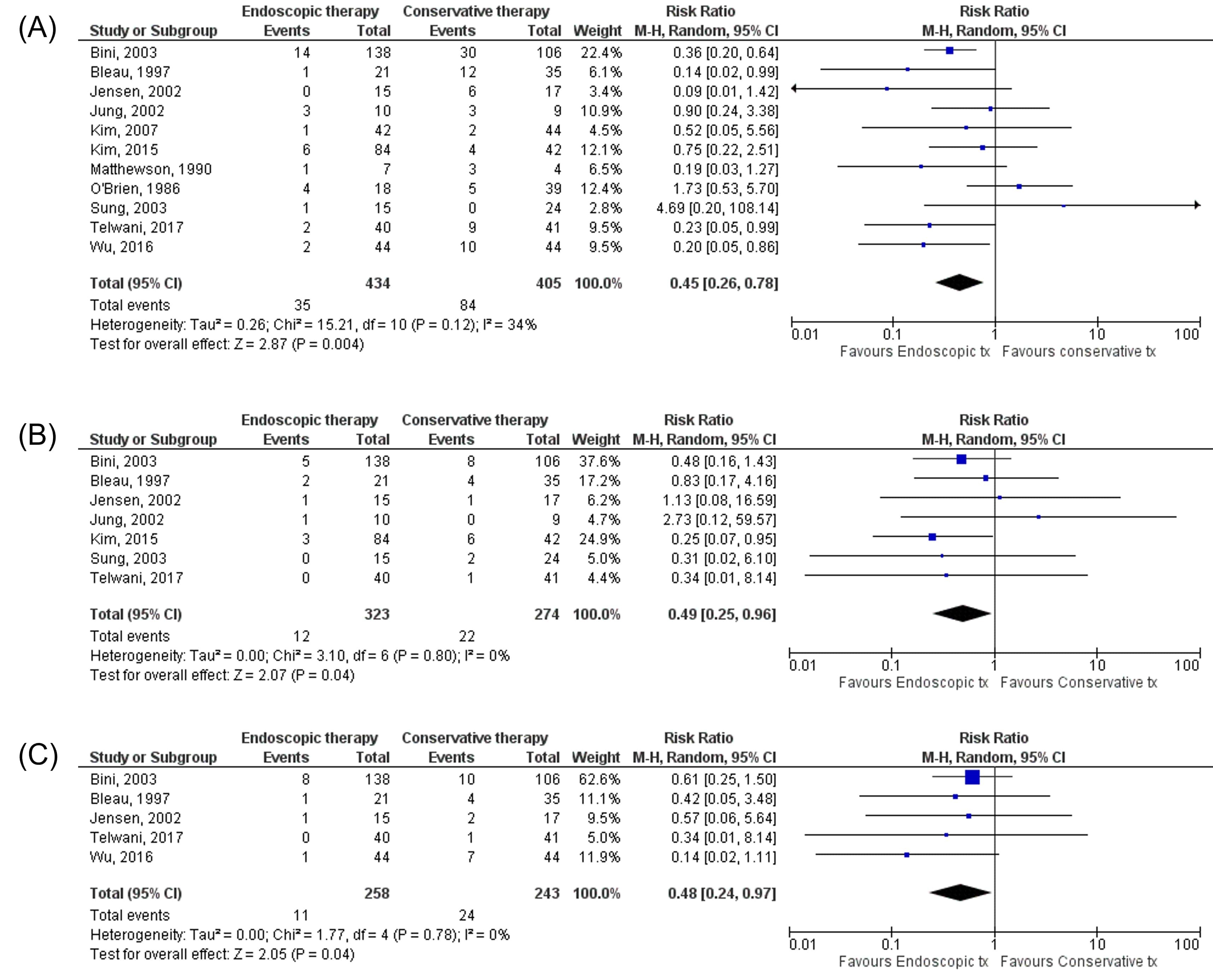
Figure: Figure 1
Disclosures:
Azizullah Beran indicated no relevant financial relationships.
Yasir Al-Abboodi indicated no relevant financial relationships.
Sami Ghazaleh indicated no relevant financial relationships.
Wasef Sayeh indicated no relevant financial relationships.
Mouhand Mohamed indicated no relevant financial relationships.
Khaled Elfert indicated no relevant financial relationships.
Rami Musallam indicated no relevant financial relationships.
Anas Alsughayer indicated no relevant financial relationships.
David Farrow indicated no relevant financial relationships.
Syed Hamaad Rahman indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified sciences – Grant/Research Support. Cook endoscopy – Grant/Research Support. Creatics LLC – Grant/Research Support.
Azizullah Beran, MD1, Yasir Al-Abboodi, MD1, Sami Ghazaleh, MD1, Wasef Sayeh, MD1, Mouhand F. Mohamed, MD, MSc2, Khaled Elfert, MD, MRCP3, Rami Musallam, MD4, Anas Alsughayer, MD5, David Farrow, MD1, Syed Hamaad Rahman, DO6, Mohammad Al-Haddad, MD, MSc7, 6, Endoscopic vs Conservative Treatment for Bleeding Peptic Ulcer With Adherent Clot: A Comprehensive Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


