Back
Oral Paper Presentation
Annual Scientific Meeting
Session: Presidential Plenary Session 2
9 - Combining Surgical Pyloroplasty and Gastric Electrical Stimulation in Gastroparetic Patients Is Superior to Pyloroplasty Alone: A Randomized Double Blind Placebo Control Trial
Monday, October 24, 2022
10:06 AM – 10:18 AM ET
Location: Hall C2

Irene Sarosiek, MD
Texas Tech University Health Sciences Center
El Paso, TX
Presenting Author(s)
Award: Outstanding Research Award in the Stomach Category
Irene Sarosiek, MD1, Ryan Torelli, 2, Mohammad Bashashati, MD1, Jesus Diaz, MD1, Oswaldo Padilla, MD1, Bright Tamis, MD1, Sherif E. Elhanafi, MD1, Brian Davis, MD1, Richard W. McCallum, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2Paul L. Foster School of Medicine, El Paso, TX
Introduction: Pathophysiology of gastroparesis (GP) is related to the depletion of interstitial cells of Cajal in the stomach and suspected pathology of the pyloric smooth muscle. Pyloroplasty (PP) accelerates gastric emptying (GE), while gastric electrical stimulation (GES) improves GP symptoms. Our double-blind randomized clinical trial investigated if combining surgical PP and GES is more effective than PP alone.
Methods: Drug refractory GP patients underwent simultaneous surgical implantation of the GES system with PP. Scintigraphic GE was performed at baseline (all participants were delayed at 4 h with >10 % retention), and 3 months after surgery. Patients were randomized to 3 months of active GES stimulation (ON group with default setting of GES parameters), or no stimulation (OFF group). All patients then had GES turned ON for another 3 months. GP Cardinal Symptom Index (GCSI) with 6-points scale (0- none; 5-very severe) was recorded at baseline, 3 and 6 months after the surgery. Delta changes of GCSI and individual GP symptoms in ON and OFF groups at 3 and 6 months versus their baseline were calculated and compared using two-way ANOVA followed by Tukey’s post-hoc analysis.
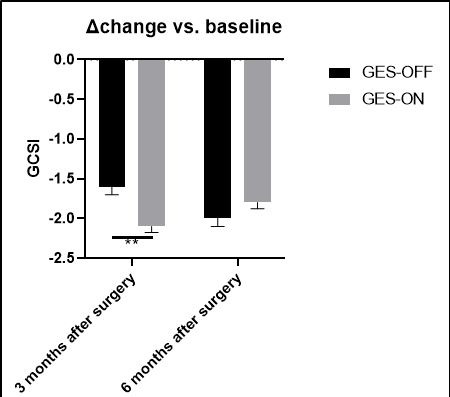
Results: 30 GP patients (18F; mean age 46 (21-72); 6 idiopathics; 24 diabetics with mean duration of DM 24 years (3-50); mean duration of GP 5.6 (1-18) years met criteria for the trial. The mean baseline 4 h GE retention was not different in GES-OFF and -ON group. GE was significantly accelerated at 3 months in GES-OFF (46%) and GES-ON (62%) groups (*p < 0.05), and 39% patients normalized their 4h GE. Patients were randomized to GES-OFF or ON (15 patients per group). GP etiologies were similar in both groups. Baseline GCSI in GES-OFF (3.5±0.2) was comparable to GES-ON (3.7±0.2) group, and significantly improved in 3 months compared to baseline (p < 0.01) in both groups. However, mean GCSI score was significantly better (p < 0.05) in GES-ON than GES-OFF group (Figure 1). When GES was turned ON in GES-OFF group at 3 months their GSCI significantly improved at 6 months. The frequency of hospitalizations due to vomiting was significantly reduced in GES-ON vs. OFF group (p=0.02). There were no post-surgical complications or technical dysfunctions recorded during this trial.
Discussion: Our randomized, double-blind study has revealed for the first time that combining GES with pyloroplasty is statistically more effective than PP alone in controlling GP symptoms and GE is similarly accelerated following PP in both groups.
Disclosures:
Irene Sarosiek, MD1, Ryan Torelli, 2, Mohammad Bashashati, MD1, Jesus Diaz, MD1, Oswaldo Padilla, MD1, Bright Tamis, MD1, Sherif E. Elhanafi, MD1, Brian Davis, MD1, Richard W. McCallum, MD1, 9, Combining Surgical Pyloroplasty and Gastric Electrical Stimulation in Gastroparetic Patients Is Superior to Pyloroplasty Alone: A Randomized Double Blind Placebo Control Trial, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Irene Sarosiek, MD1, Ryan Torelli, 2, Mohammad Bashashati, MD1, Jesus Diaz, MD1, Oswaldo Padilla, MD1, Bright Tamis, MD1, Sherif E. Elhanafi, MD1, Brian Davis, MD1, Richard W. McCallum, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2Paul L. Foster School of Medicine, El Paso, TX
Introduction: Pathophysiology of gastroparesis (GP) is related to the depletion of interstitial cells of Cajal in the stomach and suspected pathology of the pyloric smooth muscle. Pyloroplasty (PP) accelerates gastric emptying (GE), while gastric electrical stimulation (GES) improves GP symptoms. Our double-blind randomized clinical trial investigated if combining surgical PP and GES is more effective than PP alone.
Methods: Drug refractory GP patients underwent simultaneous surgical implantation of the GES system with PP. Scintigraphic GE was performed at baseline (all participants were delayed at 4 h with >10 % retention), and 3 months after surgery. Patients were randomized to 3 months of active GES stimulation (ON group with default setting of GES parameters), or no stimulation (OFF group). All patients then had GES turned ON for another 3 months. GP Cardinal Symptom Index (GCSI) with 6-points scale (0- none; 5-very severe) was recorded at baseline, 3 and 6 months after the surgery. Delta changes of GCSI and individual GP symptoms in ON and OFF groups at 3 and 6 months versus their baseline were calculated and compared using two-way ANOVA followed by Tukey’s post-hoc analysis.
Results: 30 GP patients (18F; mean age 46 (21-72); 6 idiopathics; 24 diabetics with mean duration of DM 24 years (3-50); mean duration of GP 5.6 (1-18) years met criteria for the trial. The mean baseline 4 h GE retention was not different in GES-OFF and -ON group. GE was significantly accelerated at 3 months in GES-OFF (46%) and GES-ON (62%) groups (*p < 0.05), and 39% patients normalized their 4h GE. Patients were randomized to GES-OFF or ON (15 patients per group). GP etiologies were similar in both groups. Baseline GCSI in GES-OFF (3.5±0.2) was comparable to GES-ON (3.7±0.2) group, and significantly improved in 3 months compared to baseline (p < 0.01) in both groups. However, mean GCSI score was significantly better (p < 0.05) in GES-ON than GES-OFF group (Figure 1). When GES was turned ON in GES-OFF group at 3 months their GSCI significantly improved at 6 months. The frequency of hospitalizations due to vomiting was significantly reduced in GES-ON vs. OFF group (p=0.02). There were no post-surgical complications or technical dysfunctions recorded during this trial.
Discussion: Our randomized, double-blind study has revealed for the first time that combining GES with pyloroplasty is statistically more effective than PP alone in controlling GP symptoms and GE is similarly accelerated following PP in both groups.
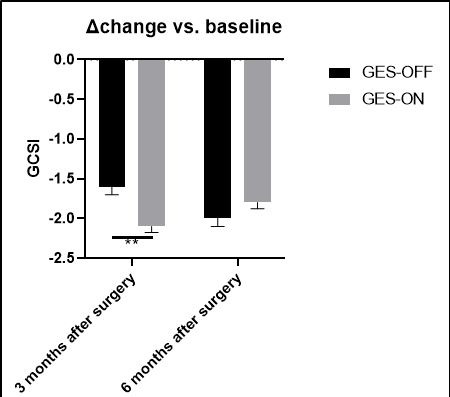
Figure: Figure 1) Changes of Gastroparesis Cardinal Symptom Index (GCSI) at 3 and 6 months in GES-ON versus GES-OFF group compared to baseline. **p < 0.01
Disclosures:
Irene Sarosiek indicated no relevant financial relationships.
Ryan Torelli indicated no relevant financial relationships.
Mohammad Bashashati indicated no relevant financial relationships.
Jesus Diaz indicated no relevant financial relationships.
Oswaldo Padilla indicated no relevant financial relationships.
Bright Tamis indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Brian Davis indicated no relevant financial relationships.
Richard McCallum indicated no relevant financial relationships.
Irene Sarosiek, MD1, Ryan Torelli, 2, Mohammad Bashashati, MD1, Jesus Diaz, MD1, Oswaldo Padilla, MD1, Bright Tamis, MD1, Sherif E. Elhanafi, MD1, Brian Davis, MD1, Richard W. McCallum, MD1, 9, Combining Surgical Pyloroplasty and Gastric Electrical Stimulation in Gastroparetic Patients Is Superior to Pyloroplasty Alone: A Randomized Double Blind Placebo Control Trial, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.



