Back
Oral Paper Presentation
Annual Scientific Meeting
Session: Plenary Session 2B - Endoscopy / Stomach / GI Bleeding
33 - Endoscopic vs Surgical Procedures for Gastroesophageal Reflux Disease - A Network Meta-Analysis
Tuesday, October 25, 2022
9:20 AM – 9:30 AM ET
Location: Hall C1

Ravi Teja Pasam, MBBS, MPH
Lahey Hospital & Medical Center
Burlington, MA
Presenting Author(s)
Ravi Teja Pasam, MBBS, MPH1, Karim Osman, MD1, Babu P. Mohan, MD, MS2, Douglas G. Adler, MD, FACG3
1Lahey Hospital & Medical Center, Burlington, MA; 2University of Utah School of Medicine, Salt Lake City, UT; 3Centura Health-Porter Adventist Hospital, Salt Lake City, UT
Introduction: Various surgical fundoplication (SF) procedures have been the mainstay therapy for medication refractory GERD. Over the last couple of decades, interventional endoscopic procedures such as radiofrequency energy delivery with Stretta, endoscopic fundoplication (EF) procedures with EsophyX and GERDx systems, and laparoscopic magnetic sphincter augmentation (Linx), have emerged as alternative options. Objective of our study was to compare the efficacy of these various procedures.
Methods: A comprehensive search of the available electronic databases was conducted, and only RCTs with our procedures of interest were included in our network meta-analysis using random-effects analysis. Outcomes of interest were lower esophageal sphincter pressure (LESP), esophagitis, cessation of use of proton pump inhibitors (PPIs), and percentage of time with a pH less than 4 on a 24-hour esophageal pH monitoring (% time pH< 4) at a follow-up of one year or less.
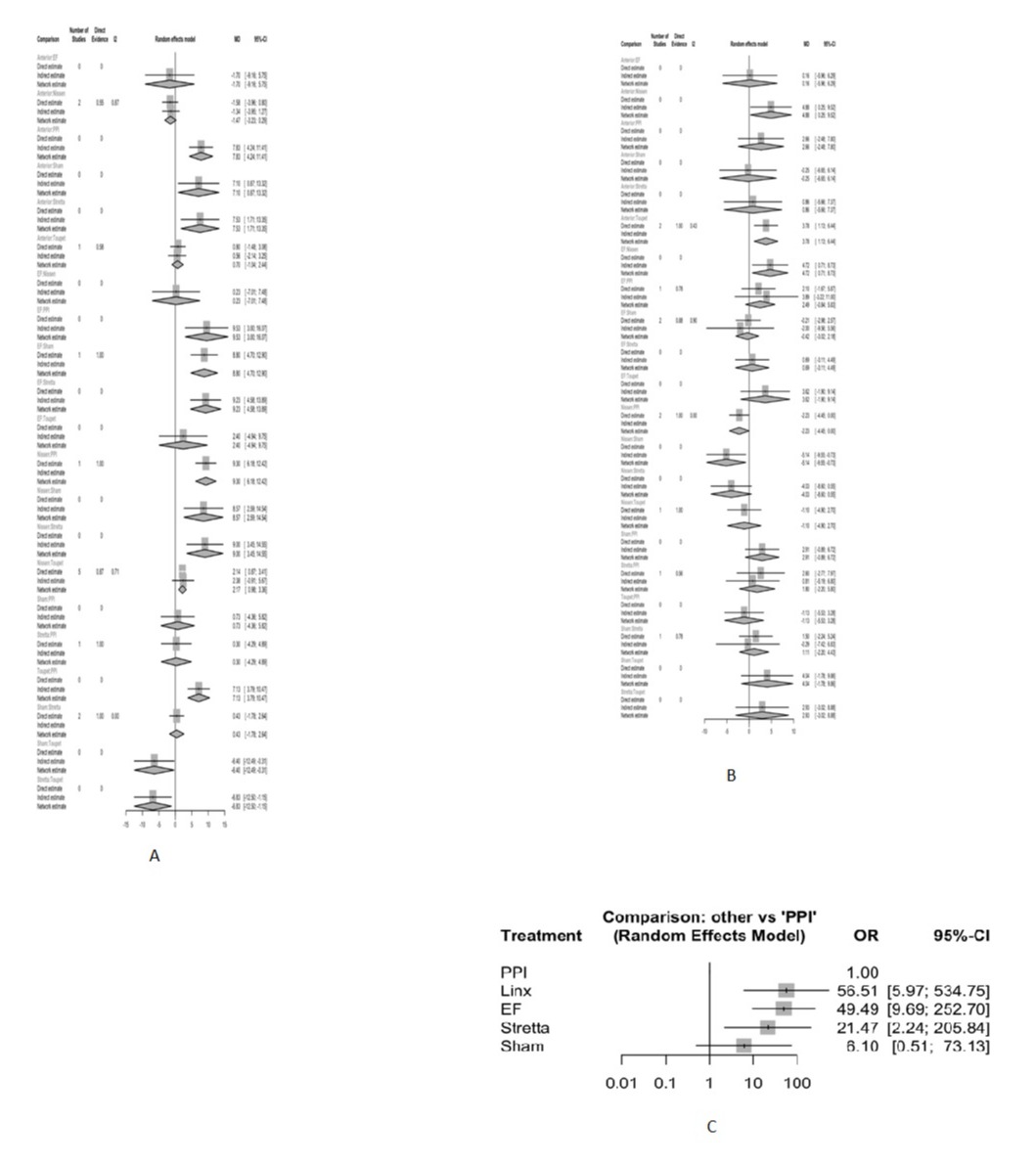
Results: Thirty-one studies with a total of 4,371 patients were included in the analysis. EF and SF were associated with significantly higher LESP compared to PPI. There was no significant difference between EF and Nissen [Mean Difference (MD): 0.23, 95%CI: -7.01-7.48], anterior (MD: 1.76, 95% CI: -5.75-9.16) or Toupet (MD: 2.4, 95%CI: -4.94-9.75) fundoplications. In contrast, Stretta was inferior to Nissen (MD: -9.00, 95%CI: -14.55 - -3.45), Toupet (MD: -6.83, 95%CI: -12.50 - -1.55) and anterior (MD: -7.5, 95%CI: -13.35 - -1.71). Regarding % time pH< 4, EF was significantly better than Nissen (MD: 4.72, 95%CI: 0.71-8.73), but not significantly different from either Toupet (MD: 3.62, 95%CI: -1.90-9.14) or anterior (MD: -0.16, 95%CI: -6.29-5.96) fundoplications, and none of the procedures were significantly different from the PPI group. Cessation of PPI usage was significantly higher for endoscopic and surgical (only Linx) procedures compared to PPI group, but none of the procedures had significant differences when compared to each other. Endoscopic and surgical procedures (only SF) did not differ significantly from each other or from the PPI group in terms of presence of esophagitis at follow-up.
Discussion: Efficacy of EF seemed comparable to SF in the short-term. Stretta was found to be inferior to all procedures in terms of LESP. Further studies focusing on head to head trials between EF and SF, and long term outcomes of EF are required to understand the place of EF in the treatment hierarchy.
Disclosures:
Ravi Teja Pasam, MBBS, MPH1, Karim Osman, MD1, Babu P. Mohan, MD, MS2, Douglas G. Adler, MD, FACG3, 33, Endoscopic vs Surgical Procedures for Gastroesophageal Reflux Disease - A Network Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Lahey Hospital & Medical Center, Burlington, MA; 2University of Utah School of Medicine, Salt Lake City, UT; 3Centura Health-Porter Adventist Hospital, Salt Lake City, UT
Introduction: Various surgical fundoplication (SF) procedures have been the mainstay therapy for medication refractory GERD. Over the last couple of decades, interventional endoscopic procedures such as radiofrequency energy delivery with Stretta, endoscopic fundoplication (EF) procedures with EsophyX and GERDx systems, and laparoscopic magnetic sphincter augmentation (Linx), have emerged as alternative options. Objective of our study was to compare the efficacy of these various procedures.
Methods: A comprehensive search of the available electronic databases was conducted, and only RCTs with our procedures of interest were included in our network meta-analysis using random-effects analysis. Outcomes of interest were lower esophageal sphincter pressure (LESP), esophagitis, cessation of use of proton pump inhibitors (PPIs), and percentage of time with a pH less than 4 on a 24-hour esophageal pH monitoring (% time pH< 4) at a follow-up of one year or less.
Results: Thirty-one studies with a total of 4,371 patients were included in the analysis. EF and SF were associated with significantly higher LESP compared to PPI. There was no significant difference between EF and Nissen [Mean Difference (MD): 0.23, 95%CI: -7.01-7.48], anterior (MD: 1.76, 95% CI: -5.75-9.16) or Toupet (MD: 2.4, 95%CI: -4.94-9.75) fundoplications. In contrast, Stretta was inferior to Nissen (MD: -9.00, 95%CI: -14.55 - -3.45), Toupet (MD: -6.83, 95%CI: -12.50 - -1.55) and anterior (MD: -7.5, 95%CI: -13.35 - -1.71). Regarding % time pH< 4, EF was significantly better than Nissen (MD: 4.72, 95%CI: 0.71-8.73), but not significantly different from either Toupet (MD: 3.62, 95%CI: -1.90-9.14) or anterior (MD: -0.16, 95%CI: -6.29-5.96) fundoplications, and none of the procedures were significantly different from the PPI group. Cessation of PPI usage was significantly higher for endoscopic and surgical (only Linx) procedures compared to PPI group, but none of the procedures had significant differences when compared to each other. Endoscopic and surgical procedures (only SF) did not differ significantly from each other or from the PPI group in terms of presence of esophagitis at follow-up.
Discussion: Efficacy of EF seemed comparable to SF in the short-term. Stretta was found to be inferior to all procedures in terms of LESP. Further studies focusing on head to head trials between EF and SF, and long term outcomes of EF are required to understand the place of EF in the treatment hierarchy.
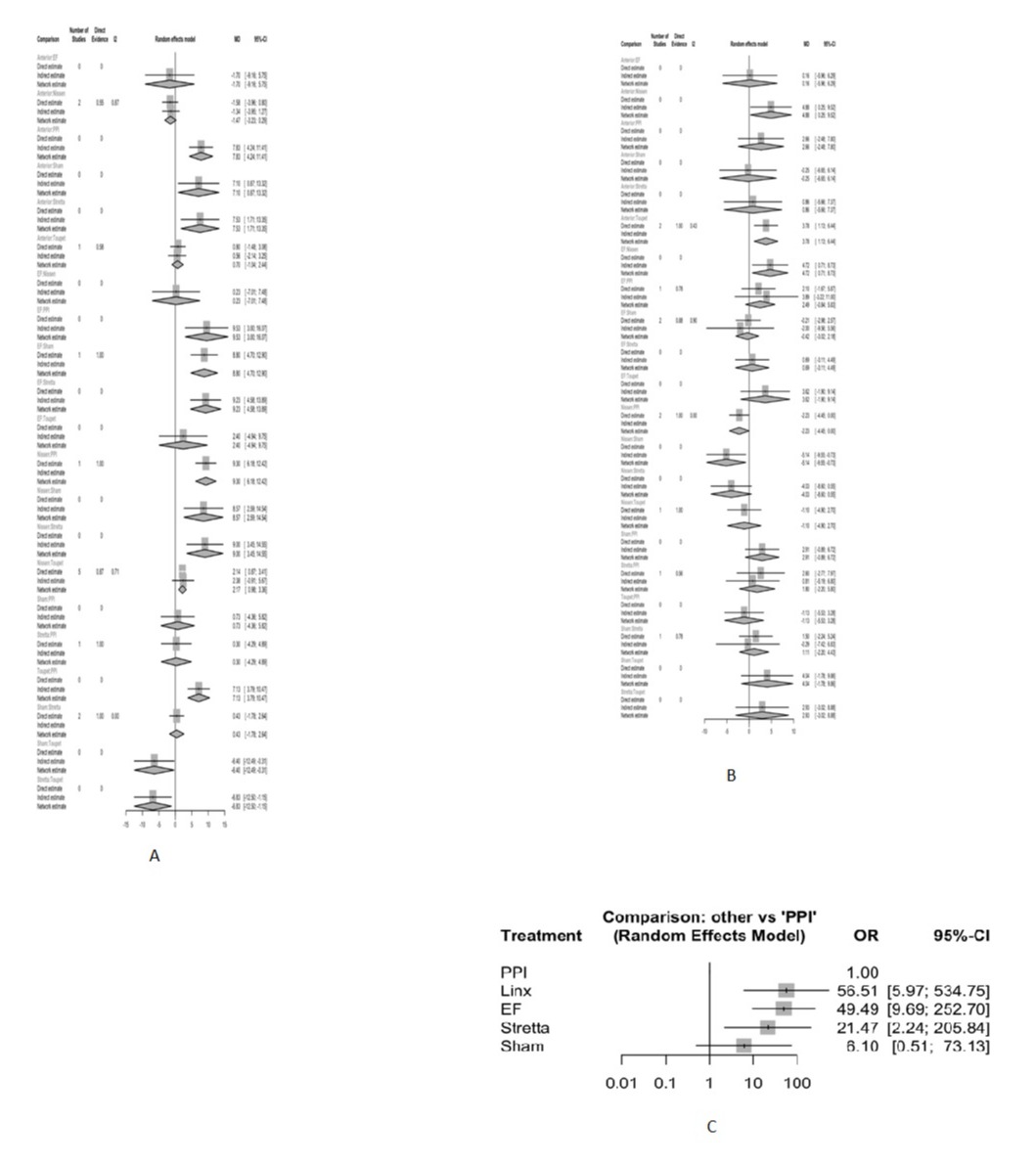
Figure: A. Direct, indirect and network estimates of post-intervention lower esophageal sphincter pressures; B. Direct, indirect and network estimates of percentage of time with a esophageal pH less than 4; C. Forest plot of cessation of PPI usage at follow-up comparing various interventions to PPI alone
Disclosures:
Ravi Teja Pasam indicated no relevant financial relationships.
Karim Osman indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Douglas Adler: Boston Scientific – Consultant.
Ravi Teja Pasam, MBBS, MPH1, Karim Osman, MD1, Babu P. Mohan, MD, MS2, Douglas G. Adler, MD, FACG3, 33, Endoscopic vs Surgical Procedures for Gastroesophageal Reflux Disease - A Network Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

