Back
Poster Session A - Sunday Afternoon
A0334 - Obesity Is Associated With an Increased Risk of Colorectal Neoplasia in Patients With Inflammatory Bowel Disease
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Benjamin I. Richter, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Benjamin I. Richter, MD1, Shaili Babbar, MD, MBA2, Tamara F. Kahan, BA3, Prabhu Sasankan, BS4, Dalia Walzer, BS5, Adam Faye, MD, MS1, Sumona Bhattacharya, MD4, Jordan Axelrad, MD, MPH4
1NYU Langone Health, New York, NY; 2New York University, Robbinsville, NJ; 3New York University, New York, NY; 4NYU Grossman School of Medicine, New York, NY; 5New York University School of Medicine, New York, NY
Introduction: Obesity is associated with an increased risk of colorectal neoplasia, but this relationship has not been studied in patients with inflammatory bowel disease (IBD). Both IBD and obesity induce a chronic inflammatory state, so the combination of the two could have an additive or synergistic effect on risk of colorectal neoplasia. Given the increased baseline incidence of dysplasia among IBD patients, identifying modifiable risk factors, such as obesity, could have a significant impact on long term cancer-related outcomes.
Methods: We performed a retrospective case-control study of IBD colitis patients at an academic IBD Center between January 2006 and February 2022. Demographic and disease-related data, known risk factors for dysplasia, and median BMI during the follow-up period were obtained. Only patients with at least 5 years of colonoscopy reports were included. A case was defined as any patient with biopsy proven dysplasia—indefinite, low-grade, or high-grade—during the study period. A control was defined as any patient with absence of biopsy-proven dysplasia. Obesity was defined as BMI of 30 or greater. Univariate analysis was performed using T-test for continuous variables and chi-square for categorical variables. Multivariate analysis was performed using logistic regression to model dysplasia risk.
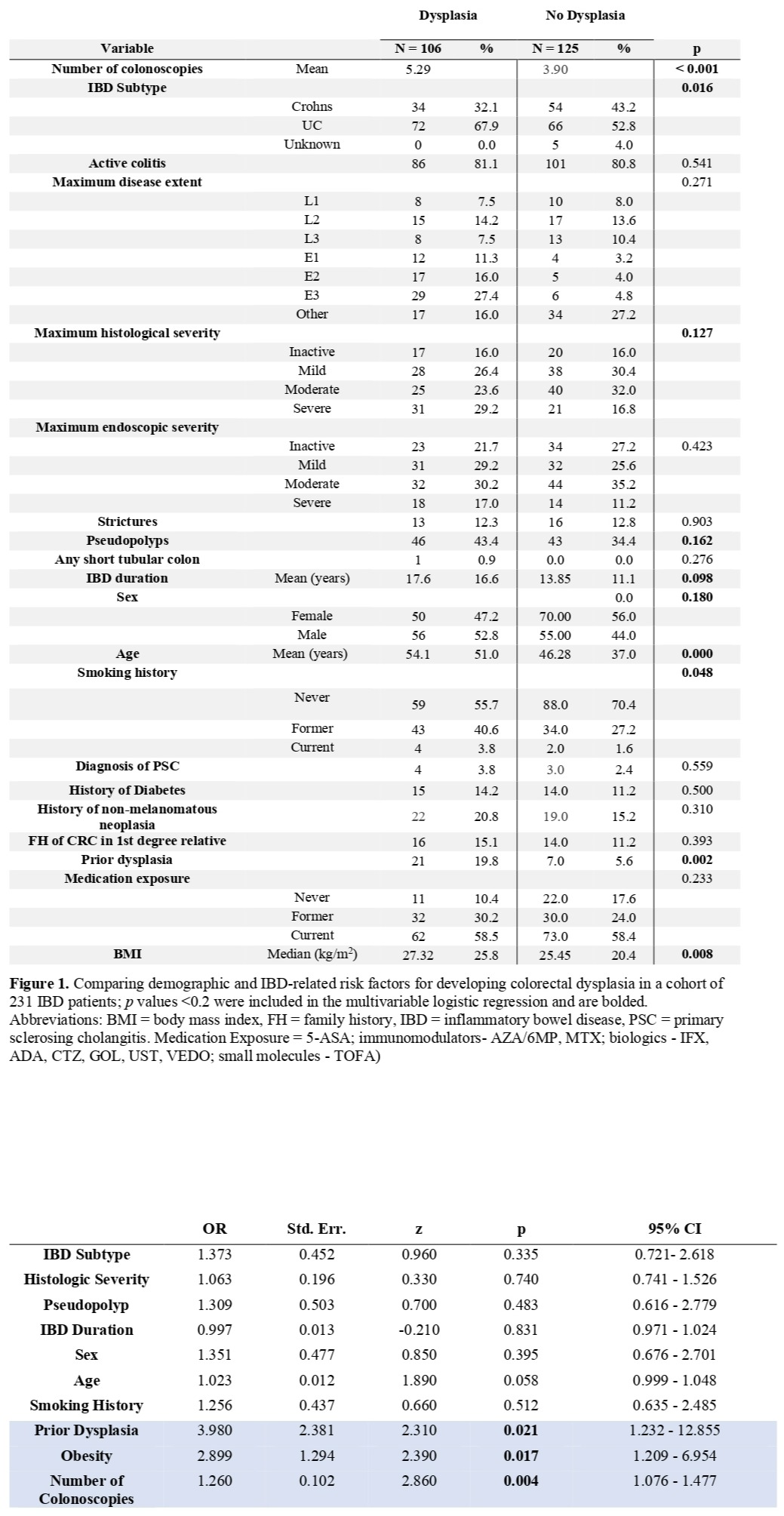
Results: 106 cases had biopsy-proven colorectal dysplasia (64 IND, 36 LGD, 10 HGD); 125 controls had no dysplasia. Number of colonoscopies (p < 0.001) IBD subtype ulcerative colitis (p = 0.016), maximum histologic severity (p = 0.127), pseudopolyps (p = 0.162), IBD duration (p = 0.098), sex (p = 0.18), age (p < 0.001), smoking history (p = 0.048), prior dysplasia (p < 0.001), and obesity (p < 0.001) were associated with dysplasia on univariate analysis. On multivariable regression, number of colonoscopies (OR 1.26, 95% CI 1.08 - 1.48, p = 0.004), prior dysplasia (OR 3.98, 95% CI 1.23 - 12.86, p = 0.021), and obesity (OR 2.90, 95% CI 1.21 - 6.95, p = 0.017) were each independently associated with increased dysplasia risk.
Discussion: Patients with IBD have an increased risk of colorectal neoplasia, but a variety of comorbid states may exacerbate this risk. Notably, we identified obesity as an independent risk factor for dysplasia. Further research is needed to determine whether this risk functions synergistically with IBD or just as an independent risk factor. Furthermore, targeted weight-loss interventions may reduce the incidence of dysplasia among patients with IBD.
Disclosures:
Benjamin I. Richter, MD1, Shaili Babbar, MD, MBA2, Tamara F. Kahan, BA3, Prabhu Sasankan, BS4, Dalia Walzer, BS5, Adam Faye, MD, MS1, Sumona Bhattacharya, MD4, Jordan Axelrad, MD, MPH4. A0334 - Obesity Is Associated With an Increased Risk of Colorectal Neoplasia in Patients With Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2New York University, Robbinsville, NJ; 3New York University, New York, NY; 4NYU Grossman School of Medicine, New York, NY; 5New York University School of Medicine, New York, NY
Introduction: Obesity is associated with an increased risk of colorectal neoplasia, but this relationship has not been studied in patients with inflammatory bowel disease (IBD). Both IBD and obesity induce a chronic inflammatory state, so the combination of the two could have an additive or synergistic effect on risk of colorectal neoplasia. Given the increased baseline incidence of dysplasia among IBD patients, identifying modifiable risk factors, such as obesity, could have a significant impact on long term cancer-related outcomes.
Methods: We performed a retrospective case-control study of IBD colitis patients at an academic IBD Center between January 2006 and February 2022. Demographic and disease-related data, known risk factors for dysplasia, and median BMI during the follow-up period were obtained. Only patients with at least 5 years of colonoscopy reports were included. A case was defined as any patient with biopsy proven dysplasia—indefinite, low-grade, or high-grade—during the study period. A control was defined as any patient with absence of biopsy-proven dysplasia. Obesity was defined as BMI of 30 or greater. Univariate analysis was performed using T-test for continuous variables and chi-square for categorical variables. Multivariate analysis was performed using logistic regression to model dysplasia risk.
Results: 106 cases had biopsy-proven colorectal dysplasia (64 IND, 36 LGD, 10 HGD); 125 controls had no dysplasia. Number of colonoscopies (p < 0.001) IBD subtype ulcerative colitis (p = 0.016), maximum histologic severity (p = 0.127), pseudopolyps (p = 0.162), IBD duration (p = 0.098), sex (p = 0.18), age (p < 0.001), smoking history (p = 0.048), prior dysplasia (p < 0.001), and obesity (p < 0.001) were associated with dysplasia on univariate analysis. On multivariable regression, number of colonoscopies (OR 1.26, 95% CI 1.08 - 1.48, p = 0.004), prior dysplasia (OR 3.98, 95% CI 1.23 - 12.86, p = 0.021), and obesity (OR 2.90, 95% CI 1.21 - 6.95, p = 0.017) were each independently associated with increased dysplasia risk.
Discussion: Patients with IBD have an increased risk of colorectal neoplasia, but a variety of comorbid states may exacerbate this risk. Notably, we identified obesity as an independent risk factor for dysplasia. Further research is needed to determine whether this risk functions synergistically with IBD or just as an independent risk factor. Furthermore, targeted weight-loss interventions may reduce the incidence of dysplasia among patients with IBD.
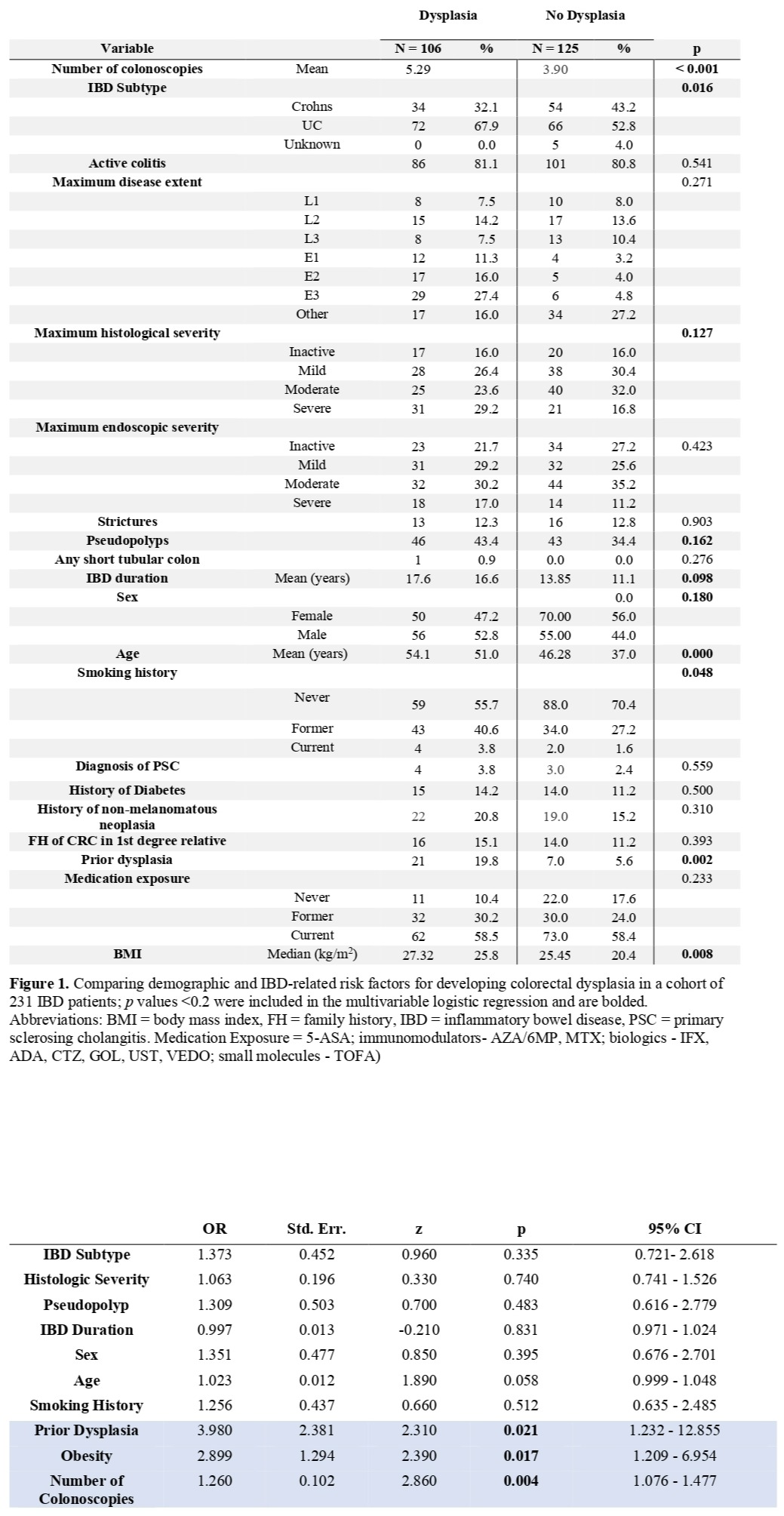
Figure: Univariate Analysis and Multivariable Regression of Risk Factors for Dysplasia in IBD Patients
Disclosures:
Benjamin Richter indicated no relevant financial relationships.
Shaili Babbar indicated no relevant financial relationships.
Tamara Kahan indicated no relevant financial relationships.
Prabhu Sasankan indicated no relevant financial relationships.
Dalia Walzer indicated no relevant financial relationships.
Adam Faye: GLG – Consultant. Guidepoint – Consultant. Janssen – Consultant. LEK – Consultant. M3 Consulting – Consultant.
Sumona Bhattacharya indicated no relevant financial relationships.
Jordan Axelrad: AbbVie – Consultant. BioFire Diagnostics – Consultant, Grant/Research Support. BMS – Consultant. Janssen – Consultant. Pfizer – Consultant.
Benjamin I. Richter, MD1, Shaili Babbar, MD, MBA2, Tamara F. Kahan, BA3, Prabhu Sasankan, BS4, Dalia Walzer, BS5, Adam Faye, MD, MS1, Sumona Bhattacharya, MD4, Jordan Axelrad, MD, MPH4. A0334 - Obesity Is Associated With an Increased Risk of Colorectal Neoplasia in Patients With Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
