Back
Poster Session D - Tuesday Morning
D0396 - Causes of Mortality Among Hospitalized Patients With Inflammatory Bowel Disease: A Nationwide Analysis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Laura Maas, MD
Johns Hopkins Medicine
Baltimore, MD
Presenting Author(s)
Laura Maas, MD1, Andrew T. Weber, MD2, Jenny Sauk, MD3, Alyssa M. Parian, MD4, Berkeley Limketkai, MD, PhD5
1Johns Hopkins Medicine, Baltimore, MD; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3University of California, Los Angeles, Los Angeles, CA; 4Johns Hopkins, Baltimore, MD; 5UCLA School of Medicine, Los Angeles, CA
Introduction: Inflammatory bowel diseases (IBD) are chronic inflammatory disorders of the gastrointestinal tract. Data are limited whether IBD leads to an increased risk of death. This study aims to compare mean ages and causes of death between patients with vs. without IBD.
Methods: A retrospective analysis of 2010-2018 data from the National Readmissions Database (NRD) was performed. We identified IBD patients and all associated diagnoses using ICD-9/10 codes. We compared the mean ages of death, identified the most common causes of mortality, and evaluated risk of death from known IBD-related complications in IBD vs. non-IBD patients. Chi-squared tests with Rao-Scott modification were used to compare the frequencies of specific causes of mortality.
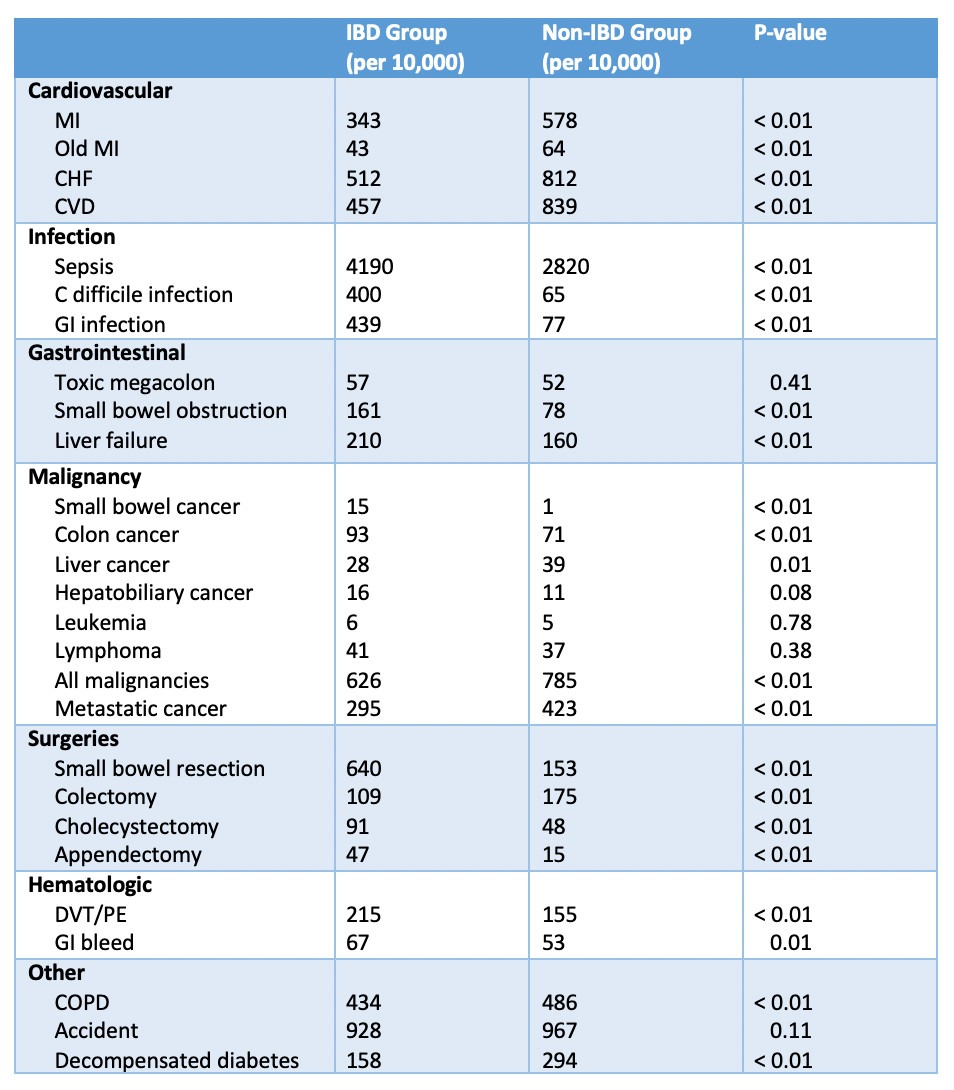
Results: There were 46,545 IBD patients and 6,344,953 non-IBD patients who died. Mean ages of death were 70.0 and 70.4 years, respectively (p<0.01). Among all causes of mortality, sepsis was the most common for both groups and was significantly higher in the IBD group (41.9% vs. 28.2%, p<0.01) (Table). The IBD group had significantly greater mortality associated with deep venous thrombosis and pulmonary embolism (DVT/PE) (2.1% vs. 1.6%, p<0.01), small bowel obstruction (1.6% vs. 0.8%, p<0.01), gastrointestinal infections (4.4% vs. 0.8%, p<0.01), C. difficile infection (4.0% vs. 0.7%, p<0.01), and gastrointestinal bleeding (0.7% vs. 0.5%, p=0.01). In addition, IBD patients had higher rates of deaths with colon cancer (0.9% vs. 0.7%, p<0.01) and small bowel cancer (0.14% vs. 0.03%, p<0.01), however deaths from leukemia, lymphoma, and hepatobiliary cancer were similar between both groups. The death rate was significantly higher in the IBD group in multiple categories of abdominal surgeries, including colectomy (10.9% vs. 1.7%, p<0.01), small bowel resection (6.4% vs. 1.5%, p<0.01), cholecystectomy (0.9% vs. 0.5%, p<0.01), and appendectomy (0.5% vs. 0.1%, p<0.01).
Discussion: The mean age of death in IBD patients was statistically higher; however, the absolute difference was only 5.2 months and thus not clinically significant. Sepsis was the leading identified cause of mortality in the two groups and was significantly higher in the IBD group. Other significant and important causes of death in IBD patients compared with non-IBD patients included C. difficile and GI infections, small bowel and colon cancers, and DVT/PE. These data can guide our efforts in preventative care, screening, and practice improvements for our IBD patients.
Disclosures:
Laura Maas, MD1, Andrew T. Weber, MD2, Jenny Sauk, MD3, Alyssa M. Parian, MD4, Berkeley Limketkai, MD, PhD5. D0396 - Causes of Mortality Among Hospitalized Patients With Inflammatory Bowel Disease: A Nationwide Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Johns Hopkins Medicine, Baltimore, MD; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3University of California, Los Angeles, Los Angeles, CA; 4Johns Hopkins, Baltimore, MD; 5UCLA School of Medicine, Los Angeles, CA
Introduction: Inflammatory bowel diseases (IBD) are chronic inflammatory disorders of the gastrointestinal tract. Data are limited whether IBD leads to an increased risk of death. This study aims to compare mean ages and causes of death between patients with vs. without IBD.
Methods: A retrospective analysis of 2010-2018 data from the National Readmissions Database (NRD) was performed. We identified IBD patients and all associated diagnoses using ICD-9/10 codes. We compared the mean ages of death, identified the most common causes of mortality, and evaluated risk of death from known IBD-related complications in IBD vs. non-IBD patients. Chi-squared tests with Rao-Scott modification were used to compare the frequencies of specific causes of mortality.
Results: There were 46,545 IBD patients and 6,344,953 non-IBD patients who died. Mean ages of death were 70.0 and 70.4 years, respectively (p<0.01). Among all causes of mortality, sepsis was the most common for both groups and was significantly higher in the IBD group (41.9% vs. 28.2%, p<0.01) (Table). The IBD group had significantly greater mortality associated with deep venous thrombosis and pulmonary embolism (DVT/PE) (2.1% vs. 1.6%, p<0.01), small bowel obstruction (1.6% vs. 0.8%, p<0.01), gastrointestinal infections (4.4% vs. 0.8%, p<0.01), C. difficile infection (4.0% vs. 0.7%, p<0.01), and gastrointestinal bleeding (0.7% vs. 0.5%, p=0.01). In addition, IBD patients had higher rates of deaths with colon cancer (0.9% vs. 0.7%, p<0.01) and small bowel cancer (0.14% vs. 0.03%, p<0.01), however deaths from leukemia, lymphoma, and hepatobiliary cancer were similar between both groups. The death rate was significantly higher in the IBD group in multiple categories of abdominal surgeries, including colectomy (10.9% vs. 1.7%, p<0.01), small bowel resection (6.4% vs. 1.5%, p<0.01), cholecystectomy (0.9% vs. 0.5%, p<0.01), and appendectomy (0.5% vs. 0.1%, p<0.01).
Discussion: The mean age of death in IBD patients was statistically higher; however, the absolute difference was only 5.2 months and thus not clinically significant. Sepsis was the leading identified cause of mortality in the two groups and was significantly higher in the IBD group. Other significant and important causes of death in IBD patients compared with non-IBD patients included C. difficile and GI infections, small bowel and colon cancers, and DVT/PE. These data can guide our efforts in preventative care, screening, and practice improvements for our IBD patients.
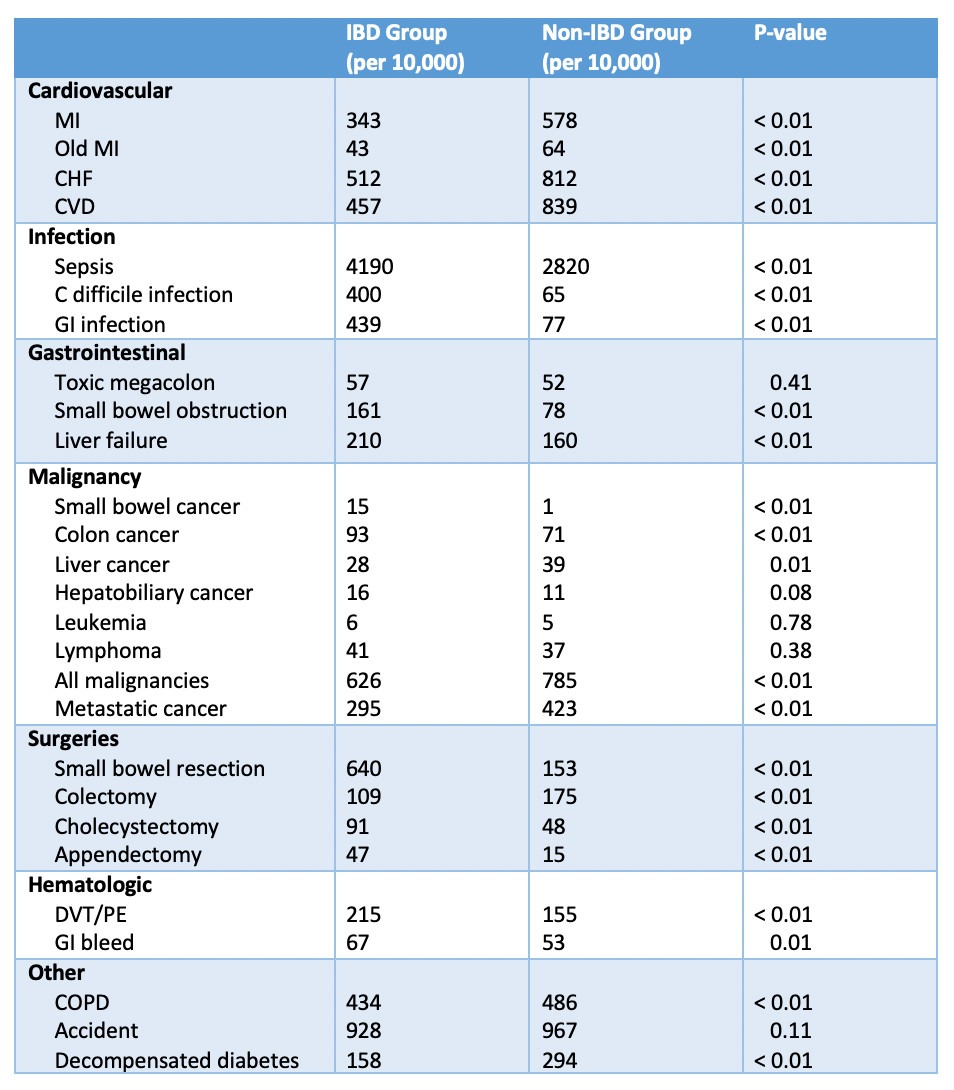
Figure: Causes of mortality in patients with and without inflammatory bowel diseases
Disclosures:
Laura Maas indicated no relevant financial relationships.
Andrew Weber indicated no relevant financial relationships.
Jenny Sauk: Abbvie – Speakers Bureau. CorEvitas – Consultant. Prometheus – Advisory Committee/Board Member.
Alyssa Parian indicated no relevant financial relationships.
Berkeley Limketkai: Azora Therapeutics – Stock-privately held company.
Laura Maas, MD1, Andrew T. Weber, MD2, Jenny Sauk, MD3, Alyssa M. Parian, MD4, Berkeley Limketkai, MD, PhD5. D0396 - Causes of Mortality Among Hospitalized Patients With Inflammatory Bowel Disease: A Nationwide Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
