Back
Poster Session A - Sunday Afternoon
A0230 - A Rare Case of Lichenoid Esophagitis Causing Refractory GERD
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Annie Shergill, MD
Larkin Community Hospital
Fresno, CA
Presenting Author(s)
Annie Shergill, MD
Larkin Community Hospital, Fresno, CA
Introduction: Lichenoid esophagitis (LE) refers to a rarely seen lichenoid pattern of inflammation in the esophagus. We report a unique case of LE in a patient with refractory gastroesophageal reflux disease (GERD) in the absence of any known risk factors that have been associated with LE.
Case Description/Methods: A 74 year old female with history of type 2 diabetes mellitus, hypertension, and GERD presented for evaluation of persistent reflux symptoms despite being on appropriate therapy with a proton pump inhibitor (PPI) for several months. Patient underwent upper endoscopy for further evaluation which showed LA grade A esophagitis without any evidence of bleeding. Esophageal biopsy showed lichenoid esophagitis pattern without any dysplasia or neoplasia. There was no evidence of CMV, HSV, or fungal infections. Patient did not have any history of cutaneous lichen planus or any rheumatological disorder. She tested negative for HIV and viral hepatitis. Her PPI dose was increased and a repeat endoscopy was scheduled in 6 months for surveillance.
Discussion: LE involves esophageal mucosal infiltration with inflammatory lymphocytes and dyskeratotic epithelial cells. It can be seen in medication-induced injury (polypharmacy), rheumatological disorders, esophageal involvement by lichen planus, viral hepatitis and HIV infections. It typically presents with esophageal strictures and dysphagia. However, it is rarely associated with refractory GERD as seen in our patient. It is prudent to recognize this histopathological entity as it has significant risk of further progression to dysplasia and neoplasia. Treatment of the underlying cause, if known may help in clinical resolution. While there are no defined guidelines currently in place, surveillance endoscopy can be valuable in the prevention of future clinical complications.
Disclosures:
Annie Shergill, MD. A0230 - A Rare Case of Lichenoid Esophagitis Causing Refractory GERD, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Larkin Community Hospital, Fresno, CA
Introduction: Lichenoid esophagitis (LE) refers to a rarely seen lichenoid pattern of inflammation in the esophagus. We report a unique case of LE in a patient with refractory gastroesophageal reflux disease (GERD) in the absence of any known risk factors that have been associated with LE.
Case Description/Methods: A 74 year old female with history of type 2 diabetes mellitus, hypertension, and GERD presented for evaluation of persistent reflux symptoms despite being on appropriate therapy with a proton pump inhibitor (PPI) for several months. Patient underwent upper endoscopy for further evaluation which showed LA grade A esophagitis without any evidence of bleeding. Esophageal biopsy showed lichenoid esophagitis pattern without any dysplasia or neoplasia. There was no evidence of CMV, HSV, or fungal infections. Patient did not have any history of cutaneous lichen planus or any rheumatological disorder. She tested negative for HIV and viral hepatitis. Her PPI dose was increased and a repeat endoscopy was scheduled in 6 months for surveillance.
Discussion: LE involves esophageal mucosal infiltration with inflammatory lymphocytes and dyskeratotic epithelial cells. It can be seen in medication-induced injury (polypharmacy), rheumatological disorders, esophageal involvement by lichen planus, viral hepatitis and HIV infections. It typically presents with esophageal strictures and dysphagia. However, it is rarely associated with refractory GERD as seen in our patient. It is prudent to recognize this histopathological entity as it has significant risk of further progression to dysplasia and neoplasia. Treatment of the underlying cause, if known may help in clinical resolution. While there are no defined guidelines currently in place, surveillance endoscopy can be valuable in the prevention of future clinical complications.
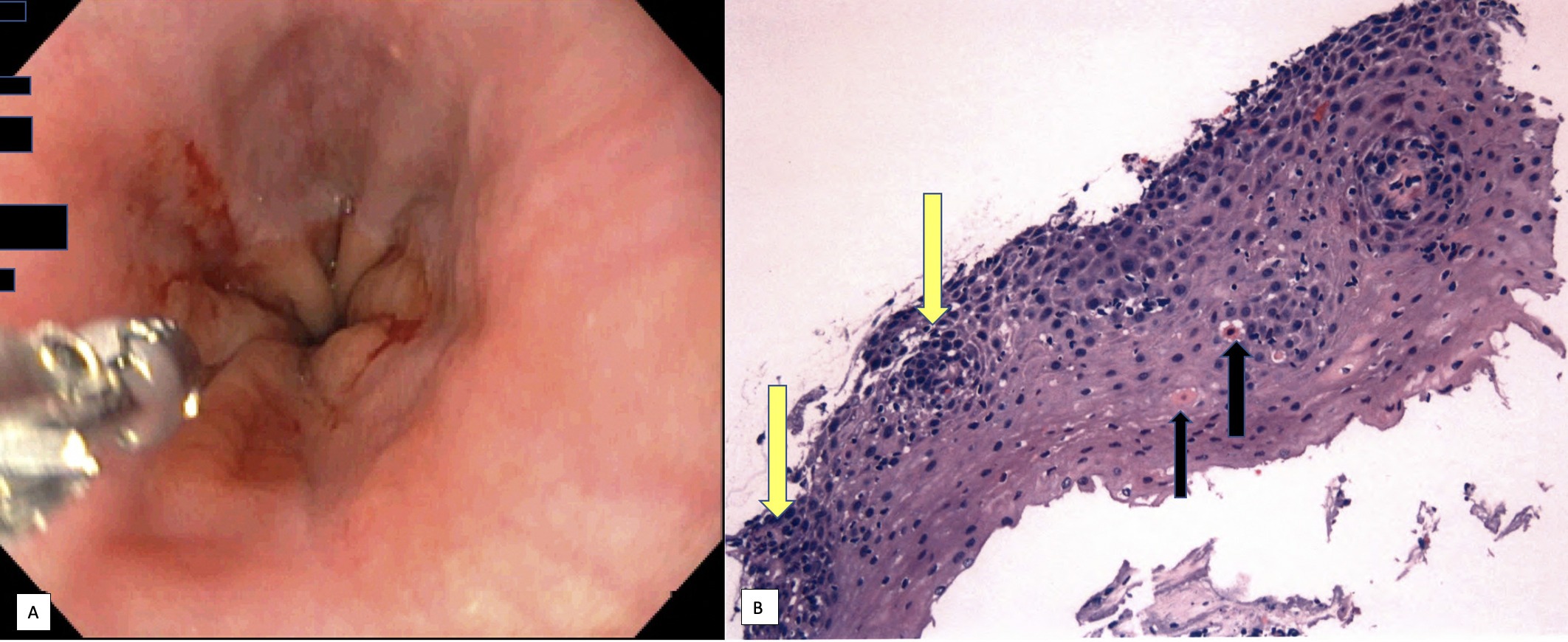
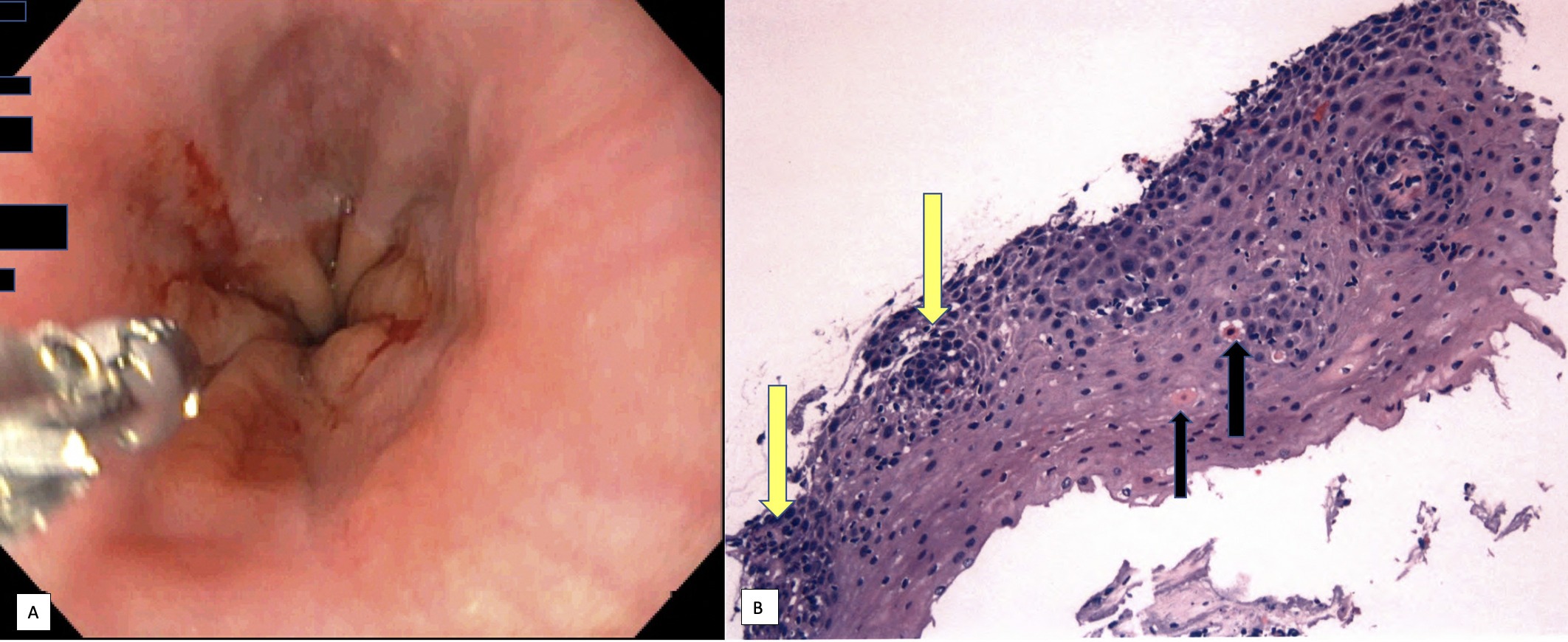
Figure: Figure 1A: Lower third of the esophagus during endoscopy showing esophagitis without any evidence of bleeding. Biopsy specimen taken and described in next image.
Figure 1B: Esophageal biopsy: squamous mucosa with a predominantly basal lymphocytic inflammatory infiltrate (yellow arrows) and associated scattered dyskeratotic epithelial cells (black arrows). No intraepithelial eosinophils are seen, no acute neutrophil-mediated inflammation is identified. No fungal organisms identified, immunohistochemistry for CMV and HSV negative. No intestinal metaplasia seen.
Figure 1B: Esophageal biopsy: squamous mucosa with a predominantly basal lymphocytic inflammatory infiltrate (yellow arrows) and associated scattered dyskeratotic epithelial cells (black arrows). No intraepithelial eosinophils are seen, no acute neutrophil-mediated inflammation is identified. No fungal organisms identified, immunohistochemistry for CMV and HSV negative. No intestinal metaplasia seen.
Disclosures:
Annie Shergill indicated no relevant financial relationships.
Annie Shergill, MD. A0230 - A Rare Case of Lichenoid Esophagitis Causing Refractory GERD, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
