Back
Poster Session D - Tuesday Morning
D0013 - Incidence, Co-Morbidities and Outcomes of Necrotising Pancreatitis in a National Inpatient Sample Database
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
.jpg)
Sarakshi Mahajan, MD
University of Arkansas
Little Rock, AR
Presenting Author(s)
Jasmeet Kaur, MD1, Siddharth Chopra, MD2, Waqas Qureshi, MD3, Sarakshi Mahajan, MD4, Rajesh Gupta, MBBS, MS5
1Temple University, Pontiac, MI; 2Saint Joseph Mercy Oakland Hospital, Pontiac, MI; 3University of Massachusetts, Worcester, MA; 4University of Arkansas, Pontiac, MI; 5Post Graduate Institute of Medical Education and Research, Chandigarh, Chandigarh, India
Introduction: Acute pancreatitis (AP) is the most common cause of gastrointestinal hospitalization in the United States and poses a significant financial burden to the healthcare system with estimated cost over 2.2 billion annually. Pancreatic necrosis develops in 10-20% of all patients with AP and is associated with increased complications, longer hospitalization with multiple readmissions and higher mortality. Aim of the study was to determine the financial burden and demographics of patients with necrotising pancreatitis.
Methods: A National representative cohort of AP patients was included between the years 2016-2019 from the National Inpatient Sample (NIS) database. Patients between ages of 18 and 90 with diagnosis AP were included in the study with stratification based on presence of necrotising pancreatitis (NP) via ICD 10 codes. Statistical analysis was done using STATA 17.0. Baseline characteristics and inpatient complications were compared between groups. Outcomes were compared after adjusting for other medical comorbidities using Elixhauser scoring. Secondary outcomes including length of stay, mortality, hospital characteristics and financial measures were compared between groups.
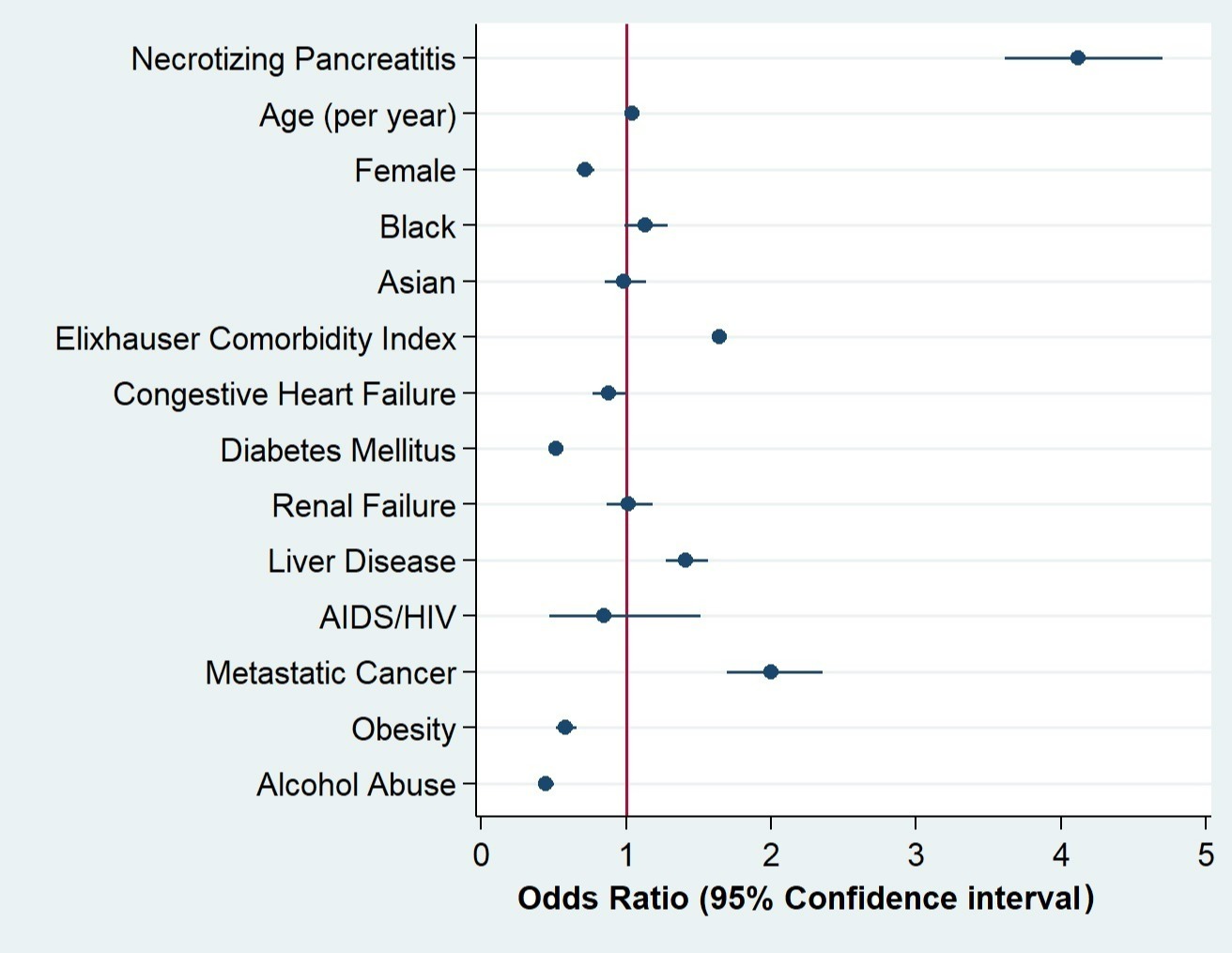
Results: Of the total, 54940 (3.5%) patients (mean age 50.4 ± 17.0 years, 35.9% females, 66.8% whites) were included in the analysis. There were no racial and gender-based differences. Mortality rates were higher among AP with necrosis than without necrosis (3.0% vs. 0.7%). AP with necrosis was independently associated with risk of mortality (OR 4.13, 95% CI 3.63 - 4.72, p < 0.001). Alcohol abuse was more common as an etiology of AP with necrosis than others (35.3% vs. 30.5%, p < 0.001). The length of stay was longer in necrosis vs. without necrosis (median LOS for AP with necrosis vs. without necrosis; 6 days vs. 3 days, p < 0.001). The cost for hospitalization was higher for NP vs. AP (median cost for AP with necrosis vs. without necrosis; $53737 vs $28531, p < 0.001). There was also a trend in the increase in the diagnosis of AP with necrosis from 2016 to 2019. Risk factors for mortality are shown in the figure.
Discussion: NP has significantly higher morbidity and mortality in individuals with AP. NP is also associated with high hospital charges and non-elective admissions.
Disclosures:
Jasmeet Kaur, MD1, Siddharth Chopra, MD2, Waqas Qureshi, MD3, Sarakshi Mahajan, MD4, Rajesh Gupta, MBBS, MS5. D0013 - Incidence, Co-Morbidities and Outcomes of Necrotising Pancreatitis in a National Inpatient Sample Database, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Temple University, Pontiac, MI; 2Saint Joseph Mercy Oakland Hospital, Pontiac, MI; 3University of Massachusetts, Worcester, MA; 4University of Arkansas, Pontiac, MI; 5Post Graduate Institute of Medical Education and Research, Chandigarh, Chandigarh, India
Introduction: Acute pancreatitis (AP) is the most common cause of gastrointestinal hospitalization in the United States and poses a significant financial burden to the healthcare system with estimated cost over 2.2 billion annually. Pancreatic necrosis develops in 10-20% of all patients with AP and is associated with increased complications, longer hospitalization with multiple readmissions and higher mortality. Aim of the study was to determine the financial burden and demographics of patients with necrotising pancreatitis.
Methods: A National representative cohort of AP patients was included between the years 2016-2019 from the National Inpatient Sample (NIS) database. Patients between ages of 18 and 90 with diagnosis AP were included in the study with stratification based on presence of necrotising pancreatitis (NP) via ICD 10 codes. Statistical analysis was done using STATA 17.0. Baseline characteristics and inpatient complications were compared between groups. Outcomes were compared after adjusting for other medical comorbidities using Elixhauser scoring. Secondary outcomes including length of stay, mortality, hospital characteristics and financial measures were compared between groups.
Results: Of the total, 54940 (3.5%) patients (mean age 50.4 ± 17.0 years, 35.9% females, 66.8% whites) were included in the analysis. There were no racial and gender-based differences. Mortality rates were higher among AP with necrosis than without necrosis (3.0% vs. 0.7%). AP with necrosis was independently associated with risk of mortality (OR 4.13, 95% CI 3.63 - 4.72, p < 0.001). Alcohol abuse was more common as an etiology of AP with necrosis than others (35.3% vs. 30.5%, p < 0.001). The length of stay was longer in necrosis vs. without necrosis (median LOS for AP with necrosis vs. without necrosis; 6 days vs. 3 days, p < 0.001). The cost for hospitalization was higher for NP vs. AP (median cost for AP with necrosis vs. without necrosis; $53737 vs $28531, p < 0.001). There was also a trend in the increase in the diagnosis of AP with necrosis from 2016 to 2019. Risk factors for mortality are shown in the figure.
Discussion: NP has significantly higher morbidity and mortality in individuals with AP. NP is also associated with high hospital charges and non-elective admissions.
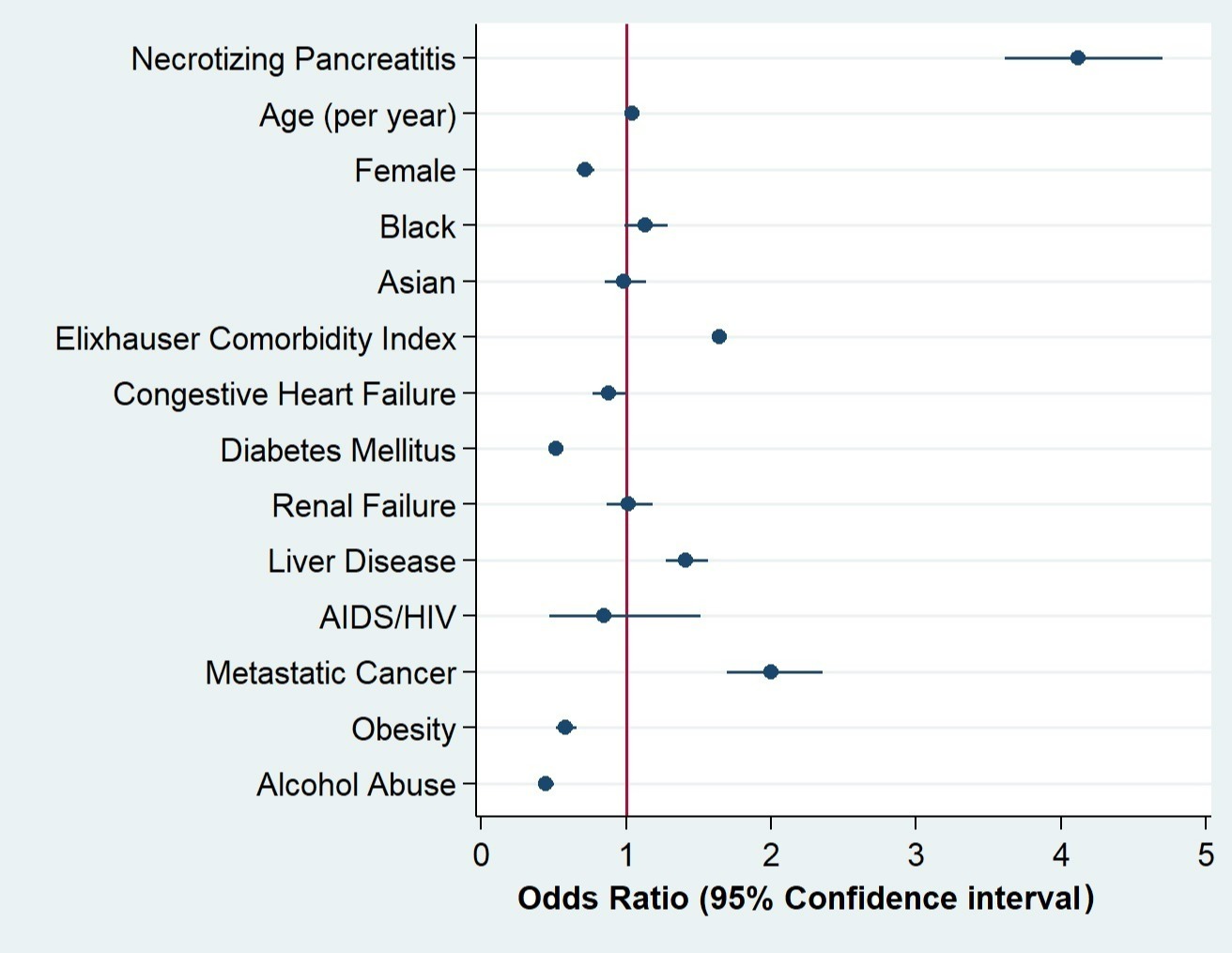
Figure: Baseline Characteristics for Necrotising pancreatitis
Disclosures:
Jasmeet Kaur indicated no relevant financial relationships.
Siddharth Chopra indicated no relevant financial relationships.
Waqas Qureshi indicated no relevant financial relationships.
Sarakshi Mahajan indicated no relevant financial relationships.
Rajesh Gupta indicated no relevant financial relationships.
Jasmeet Kaur, MD1, Siddharth Chopra, MD2, Waqas Qureshi, MD3, Sarakshi Mahajan, MD4, Rajesh Gupta, MBBS, MS5. D0013 - Incidence, Co-Morbidities and Outcomes of Necrotising Pancreatitis in a National Inpatient Sample Database, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
