Back
Poster Session D - Tuesday Morning
D0336 - Helicobacter pylori Negative Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma Presenting as a Severe Upper Gastrointestinal Bleed
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Justin L. Bilello, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Justin L. Bilello, MD, Madison Force, MD, Louis Kishfy, MD, Monjur Ahmed, MD, Alaa Hrizat, MD
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Mucosal associated lymphoid tissue lymphoma (MALT Lymphoma) is a non-Hodgkin lymphoma arising from memory B cells. H. pylori is thought to create a favorable microenvironment for neoplastic B cells, which leads to lymphoma. Surveillance and treatment of H. pylori is the only daily practice that holds clinical value in preventing gastric MALT lymphoma. As a result, the incidence of H. pylori gastric MALT lymphomas has decreased in western countries.2 At the time of diagnosis of gastrointestinal MALT lymphoma, bleeding is rarely encountered and when present, is most often occult. Here we present a unique case of H. pylori negative MALT lymphoma presenting as a severe gastrointestinal bleed.
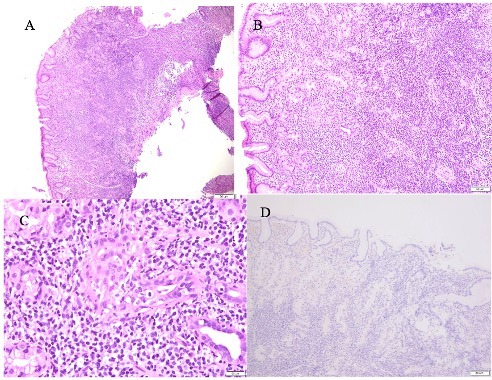
Case Description/Methods: A 75-year-old male presented after one episode of large volume melena. On initial presentation, the patient was confused and unable to provide additional history. His vital signs were significant for blood pressure of 65/28 mmHg and heart rate of 111 bpm. Labs revealed hemoglobin of 10.3 g/dL and lactate of 5.2 mmol/L. The patient was resuscitated, and a pantoprazole infusion was started. Upper endoscopy revealed a 1 cm clean-based ulcer with heaped-up margins in the gastric body. Pathology of the ulcerated tissue revealed extensive lymphoid infiltrate with atypical lymphoid cells consistent with MALT lymphoma (figure 1). Gastric antral and body biopsies were negative for H. pylori infection.
Discussion: While gastric MALT lymphoma typically presents with constitutional symptoms or dyspepsia, this case highlights an exceedingly rare presentation of H. pylori negative MALT lymphoma presenting with hemorrhagic shock. There is still much to learn about H. pylori negative MALT lymphoma, and the pathogenesis remains unclear. Identifying the pathogenesis for H. pylori negative MALT lymphomas will be paramount to improving detection and treatment options for patients. Several theories currently exist to explain the pathogenesis, including genetic alterations causing activations to nuclear factor-kappa, infection with organisms other than H. pylori, or the presence of autoimmune disease.1
1. Asano, N, et. al,. Helicobacter pylori-negative gastric mucosa-associated lymphoid tissue lymphomas: A review. 2015, 8014–8020.
2. Kiesewetter B, et. al,. Genetic Characterization and Clinical Features of Helicobacter pylori Negative Gastric Mucosa-Associated Lymphoid Tissue Lymphoma. 2021; 13(12):299
Disclosures:
Justin L. Bilello, MD, Madison Force, MD, Louis Kishfy, MD, Monjur Ahmed, MD, Alaa Hrizat, MD. D0336 - Helicobacter pylori Negative Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma Presenting as a Severe Upper Gastrointestinal Bleed, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Mucosal associated lymphoid tissue lymphoma (MALT Lymphoma) is a non-Hodgkin lymphoma arising from memory B cells. H. pylori is thought to create a favorable microenvironment for neoplastic B cells, which leads to lymphoma. Surveillance and treatment of H. pylori is the only daily practice that holds clinical value in preventing gastric MALT lymphoma. As a result, the incidence of H. pylori gastric MALT lymphomas has decreased in western countries.2 At the time of diagnosis of gastrointestinal MALT lymphoma, bleeding is rarely encountered and when present, is most often occult. Here we present a unique case of H. pylori negative MALT lymphoma presenting as a severe gastrointestinal bleed.
Case Description/Methods: A 75-year-old male presented after one episode of large volume melena. On initial presentation, the patient was confused and unable to provide additional history. His vital signs were significant for blood pressure of 65/28 mmHg and heart rate of 111 bpm. Labs revealed hemoglobin of 10.3 g/dL and lactate of 5.2 mmol/L. The patient was resuscitated, and a pantoprazole infusion was started. Upper endoscopy revealed a 1 cm clean-based ulcer with heaped-up margins in the gastric body. Pathology of the ulcerated tissue revealed extensive lymphoid infiltrate with atypical lymphoid cells consistent with MALT lymphoma (figure 1). Gastric antral and body biopsies were negative for H. pylori infection.
Discussion: While gastric MALT lymphoma typically presents with constitutional symptoms or dyspepsia, this case highlights an exceedingly rare presentation of H. pylori negative MALT lymphoma presenting with hemorrhagic shock. There is still much to learn about H. pylori negative MALT lymphoma, and the pathogenesis remains unclear. Identifying the pathogenesis for H. pylori negative MALT lymphomas will be paramount to improving detection and treatment options for patients. Several theories currently exist to explain the pathogenesis, including genetic alterations causing activations to nuclear factor-kappa, infection with organisms other than H. pylori, or the presence of autoimmune disease.1
1. Asano, N, et. al,. Helicobacter pylori-negative gastric mucosa-associated lymphoid tissue lymphomas: A review. 2015, 8014–8020.
2. Kiesewetter B, et. al,. Genetic Characterization and Clinical Features of Helicobacter pylori Negative Gastric Mucosa-Associated Lymphoid Tissue Lymphoma. 2021; 13(12):299
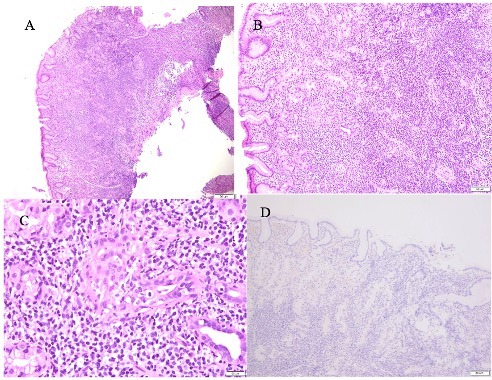
Figure: Figure 1: A) Gastric mucosa with extensive diffuse lymphoid infiltrate in lamina propria (40x). B) Destruction of gastric glands by dense lymphoplasmacytic infiltrate (100x). C) Lymphoepithelial lesions; infiltration and distortion of gastric glands by aggregates of (usually 3 or more) neoplastic lymphoid cells (400x). D) Immunostaining for H.pylori is negative (100x).
Disclosures:
Justin Bilello indicated no relevant financial relationships.
Madison Force indicated no relevant financial relationships.
Louis Kishfy indicated no relevant financial relationships.
Monjur Ahmed indicated no relevant financial relationships.
Alaa Hrizat indicated no relevant financial relationships.
Justin L. Bilello, MD, Madison Force, MD, Louis Kishfy, MD, Monjur Ahmed, MD, Alaa Hrizat, MD. D0336 - Helicobacter pylori Negative Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma Presenting as a Severe Upper Gastrointestinal Bleed, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
