Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0004 - Adherence to Most Recent Guidelines on Pancreatic Cysts Management
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Spyridon Zouridis, MD
Albany Medical Center
Albany, NY
Presenting Author(s)
Spyridon Zouridis, MD, Jacqueline Liu, , Niki Wadhwa, MD, Gurjiwan Virk, MD, Stephen Hasak, MD, MPH
Albany Medical Center, Albany, NY
Introduction: Intraductal Papillary Mucinous Neoplasms (IPMN), pseudocysts, mucinous cystic neoplasms (MCN), serous cystadenomas (SCA), other non-cancerous cysts (NoNC) are all terms describing pancreatic cysts. Some of those have been identified as pre-malignant. IPMN malignant transformation risk greatly varies depending on location, while MCN also represent potentially pre-malignant lesions, with studies showing malignancy in up to 17.5%. Pancreatic cancer is a lethal, rapidly progressive disease with low 5-year survival rate. Clear guidelines have been released to monitor pancreatic cysts, discovered incidentally on imaging, in order to identify and excise high-risk lesions prior to malignant transformation.
Methods: This is a retrospective observational cohort study, consisting of adult patients incidentally diagnosed with pancreatic cysts on imaging at our hospital from January 2016 to December 2019. Any follow-up 6 months earlier or later than the suggested time and utilization of screening methods other than the proposed were considered unsuccessful.
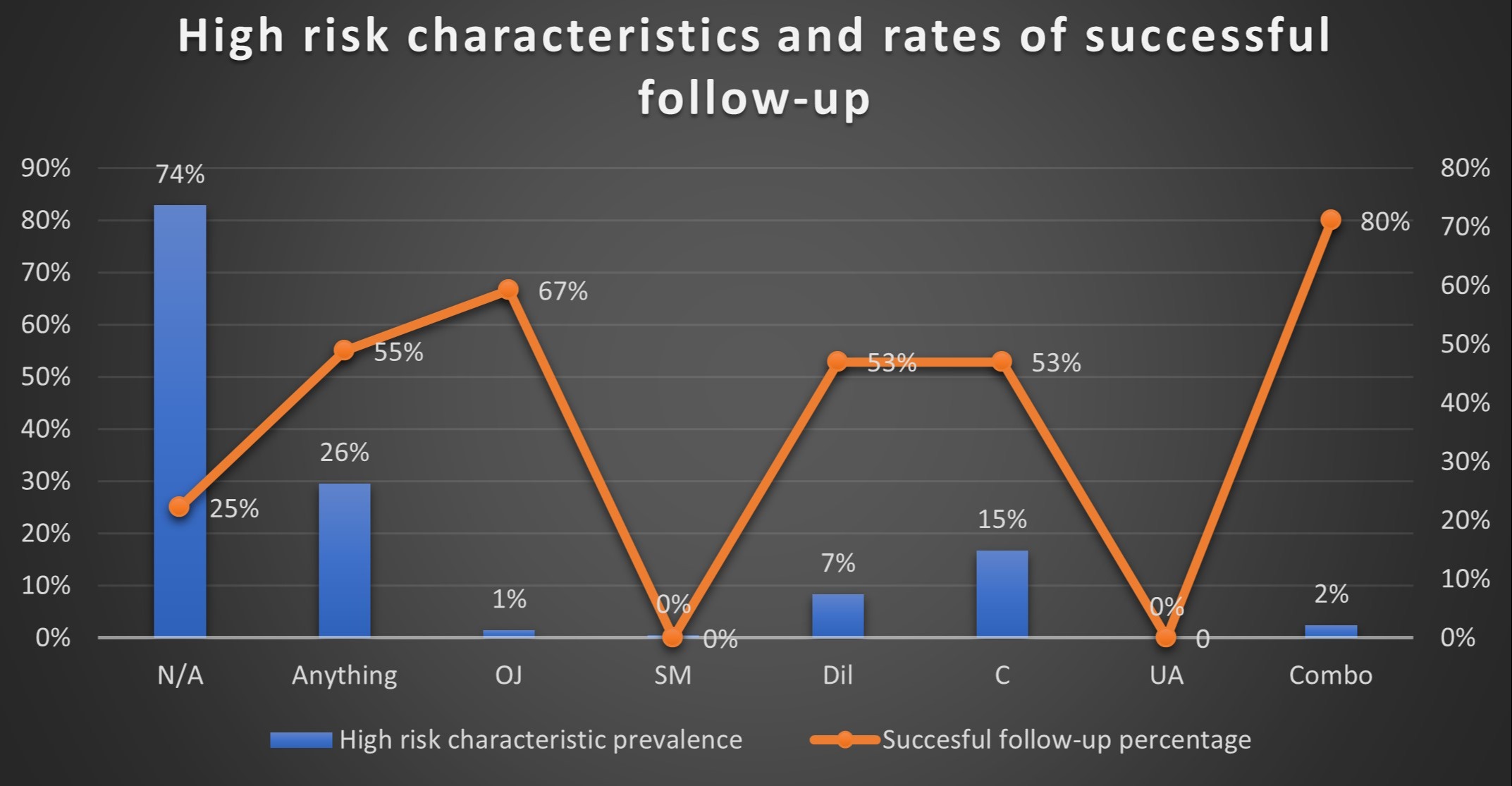
Results: Of the 228 patients included only 33% received appropriate follow-up. Patients who had a new cyst and at least one high risk characteristic on initial presentation were followed correctly in 55% of cases. Patients with more than one risk factor had even higher rates of appropriate follow-up. (Figure 1) On further analysis, the current study identifies IPMN lesions measuring < 1cm, 1-2 cm, and 2-3 cm having succesful follow-up in 16%, 35% and 53% of cases, respectively, demonstrating a clear association between the cyst size and the success of surveillance.
Discussion: Our study shows that only 33% of patients with incidentally discovered pancreatic cysts were successfully followed up based on current guidelines. Studies in the past also revealed that only around 1/3 of patients who had pancreatic cysts met minimum surveillance criteria, while presence of main pancreatic duct dilatation and absence of multiple pancreatic cysts were both associated with higher success rates. Our study confirmed that patients with any high risk characteristic had higher rates of appropriate follow-up, while the rates of successful management were directly proportional to the cyst size. Our study highlights again the gap between published guidelines and their implementation in daily practice. Additional interventions and methods for improvement should be further studied.
Disclosures:
Spyridon Zouridis, MD, Jacqueline Liu, , Niki Wadhwa, MD, Gurjiwan Virk, MD, Stephen Hasak, MD, MPH. A0004 - Adherence to Most Recent Guidelines on Pancreatic Cysts Management, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Albany Medical Center, Albany, NY
Introduction: Intraductal Papillary Mucinous Neoplasms (IPMN), pseudocysts, mucinous cystic neoplasms (MCN), serous cystadenomas (SCA), other non-cancerous cysts (NoNC) are all terms describing pancreatic cysts. Some of those have been identified as pre-malignant. IPMN malignant transformation risk greatly varies depending on location, while MCN also represent potentially pre-malignant lesions, with studies showing malignancy in up to 17.5%. Pancreatic cancer is a lethal, rapidly progressive disease with low 5-year survival rate. Clear guidelines have been released to monitor pancreatic cysts, discovered incidentally on imaging, in order to identify and excise high-risk lesions prior to malignant transformation.
Methods: This is a retrospective observational cohort study, consisting of adult patients incidentally diagnosed with pancreatic cysts on imaging at our hospital from January 2016 to December 2019. Any follow-up 6 months earlier or later than the suggested time and utilization of screening methods other than the proposed were considered unsuccessful.
Results: Of the 228 patients included only 33% received appropriate follow-up. Patients who had a new cyst and at least one high risk characteristic on initial presentation were followed correctly in 55% of cases. Patients with more than one risk factor had even higher rates of appropriate follow-up. (Figure 1) On further analysis, the current study identifies IPMN lesions measuring < 1cm, 1-2 cm, and 2-3 cm having succesful follow-up in 16%, 35% and 53% of cases, respectively, demonstrating a clear association between the cyst size and the success of surveillance.
Discussion: Our study shows that only 33% of patients with incidentally discovered pancreatic cysts were successfully followed up based on current guidelines. Studies in the past also revealed that only around 1/3 of patients who had pancreatic cysts met minimum surveillance criteria, while presence of main pancreatic duct dilatation and absence of multiple pancreatic cysts were both associated with higher success rates. Our study confirmed that patients with any high risk characteristic had higher rates of appropriate follow-up, while the rates of successful management were directly proportional to the cyst size. Our study highlights again the gap between published guidelines and their implementation in daily practice. Additional interventions and methods for improvement should be further studied.
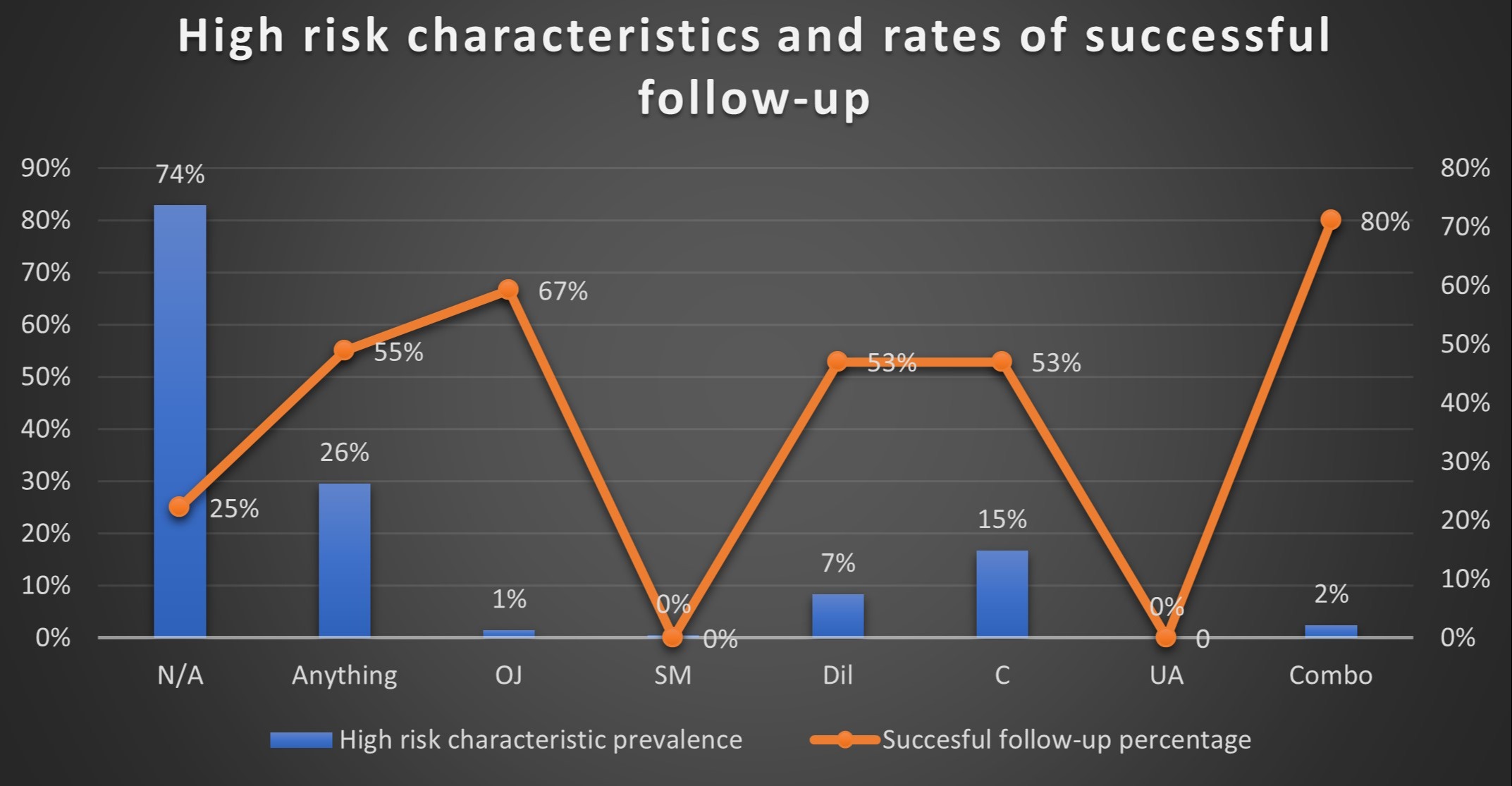
Figure: Figure 1 (N/A: No high-risk characteristic, Anything: Any high-risk characteristic, OJ: Obstructive Jaundice, SM: Associated Solid Mass presence, Dil: Main pancreatic duct diameter>5mm, C: Cyst size>3cm, UA: Change in main duct caliber with upstream atrophy, Combo: Combination of one or more high-risk characteristics)
Disclosures:
Spyridon Zouridis indicated no relevant financial relationships.
Jacqueline Liu indicated no relevant financial relationships.
Niki Wadhwa indicated no relevant financial relationships.
Gurjiwan Virk indicated no relevant financial relationships.
Stephen Hasak indicated no relevant financial relationships.
Spyridon Zouridis, MD, Jacqueline Liu, , Niki Wadhwa, MD, Gurjiwan Virk, MD, Stephen Hasak, MD, MPH. A0004 - Adherence to Most Recent Guidelines on Pancreatic Cysts Management, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
