Back

Poster Session A - Sunday Afternoon
Category: Stomach
A0715 - A Rare Case of Malignant Melanoma of the Stomach
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Aastha Bharwad, MD
The University of Kansas
Wichita, KS
Presenting Author(s)
Aastha Bharwad, MD1, Hamna Shah, MD2, William J. Salyers, MD, MPH3
1The University of Kansas, Wichita, KS; 2KU School of Medicine, Wichita, KS; 3University of Kansas, Wichita, KS
Introduction: Malignant melanoma with metastasis to the stomach is rare and seldom diagnosed before death. The most common gastrointestinal (GI) metastatic sites are the small intestine, followed by the colon, rectum, and stomach. We present the case of a 55-year-old female with a history of melanoma who presented with melena, and syncope and was found to have metastatic gastric melanoma.
Case Description/Methods: A 55-year-old female with a history of right eye choroidal melanoma (status post enucleation of the right eye) with metastasis to liver, bone, and lungs and on therapy with daily trametinib for two years presented to our hospital with chief complaints of hematochezia, fatigue, dizziness, and abdominal pain of one day. Computed Tomography Angiography (CTA) abdomen showed a small area of active bleeding at the gastroesophageal junction (GEJ). The patient was admitted to intensive care unit and was started on intravenous proton pump inhibitors, octreotide, and pressor support. Post admission, she did not report any further episodes of overt GI bleed.
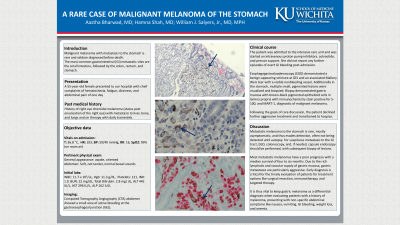
Esophagogastroduodenoscopy (EGD) demonstrated a benign-appearing stricture at GEJ and an associated Mallory Weis tear with a visible nonbleeding vessel. Additionally in the stomach, multiple small, pigmented lesions were visualized and biopsied. Biopsy demonstrated gastric mucosa with brown-black pigmented epithelioid cells in lamina propria with immunochemistry stain positive for S-100, and MART-1, diagnostic of malignant melanoma (Figure 1).
Following goals of care discussion, the patient declined further aggressive treatment and transitioned to hospice.
Discussion: Metastatic melanoma to the stomach is rare, mostly asymptomatic, and thus evades detection, often not being detected until autopsy. For suspicious metastasis to the GI tract, EGD, colonoscopy, and, if needed, capsule endoscopy should be performed, with subsequent biopsy of lesions. Most metastatic melanomas have a poor prognosis with a median survival of four to six months. Due to the rich lymphatic and vascular supply of gastric mucosa, gastric metastases are particularly aggressive. Early diagnosis is critical for the timely evaluation of patients for treatment options like surgical resection, immunotherapy, and targeted therapy. It is thus vital to keep gastric melanoma as a differential diagnosis when evaluating patients with a history of melanoma, presenting with non-specific abdominal symptoms like nausea, vomiting, GI bleeding, weight loss, and anemia.

Disclosures:
Aastha Bharwad, MD1, Hamna Shah, MD2, William J. Salyers, MD, MPH3. A0715 - A Rare Case of Malignant Melanoma of the Stomach, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1The University of Kansas, Wichita, KS; 2KU School of Medicine, Wichita, KS; 3University of Kansas, Wichita, KS
Introduction: Malignant melanoma with metastasis to the stomach is rare and seldom diagnosed before death. The most common gastrointestinal (GI) metastatic sites are the small intestine, followed by the colon, rectum, and stomach. We present the case of a 55-year-old female with a history of melanoma who presented with melena, and syncope and was found to have metastatic gastric melanoma.
Case Description/Methods: A 55-year-old female with a history of right eye choroidal melanoma (status post enucleation of the right eye) with metastasis to liver, bone, and lungs and on therapy with daily trametinib for two years presented to our hospital with chief complaints of hematochezia, fatigue, dizziness, and abdominal pain of one day. Computed Tomography Angiography (CTA) abdomen showed a small area of active bleeding at the gastroesophageal junction (GEJ). The patient was admitted to intensive care unit and was started on intravenous proton pump inhibitors, octreotide, and pressor support. Post admission, she did not report any further episodes of overt GI bleed.
Esophagogastroduodenoscopy (EGD) demonstrated a benign-appearing stricture at GEJ and an associated Mallory Weis tear with a visible nonbleeding vessel. Additionally in the stomach, multiple small, pigmented lesions were visualized and biopsied. Biopsy demonstrated gastric mucosa with brown-black pigmented epithelioid cells in lamina propria with immunochemistry stain positive for S-100, and MART-1, diagnostic of malignant melanoma (Figure 1).
Following goals of care discussion, the patient declined further aggressive treatment and transitioned to hospice.
Discussion: Metastatic melanoma to the stomach is rare, mostly asymptomatic, and thus evades detection, often not being detected until autopsy. For suspicious metastasis to the GI tract, EGD, colonoscopy, and, if needed, capsule endoscopy should be performed, with subsequent biopsy of lesions. Most metastatic melanomas have a poor prognosis with a median survival of four to six months. Due to the rich lymphatic and vascular supply of gastric mucosa, gastric metastases are particularly aggressive. Early diagnosis is critical for the timely evaluation of patients for treatment options like surgical resection, immunotherapy, and targeted therapy. It is thus vital to keep gastric melanoma as a differential diagnosis when evaluating patients with a history of melanoma, presenting with non-specific abdominal symptoms like nausea, vomiting, GI bleeding, weight loss, and anemia.

Figure: Figure 1: Gastric mucosa with brown-black pigmented epithelioid cells in lamina propria, diagnostic of malignant melanoma.
Disclosures:
Aastha Bharwad indicated no relevant financial relationships.
Hamna Shah indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
Aastha Bharwad, MD1, Hamna Shah, MD2, William J. Salyers, MD, MPH3. A0715 - A Rare Case of Malignant Melanoma of the Stomach, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
