Back

Poster Session B - Monday Morning
Category: IBD
B0362 - Impact of Early Biologic Therapy in Real-World Cohort of Crohn’s Disease Patients
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Michael Craig, MD
Brooke Army Medical Center
San Antonio, Texas
Presenting Author(s)
Michael Craig, MD1, Cody Ashcroft, MD2, David Dulaney, MD2, Robert Byrne, MD2, Thomas Weiss, MD2, Cindy Theigs, RPH3, Jodi H. Walker, BS, PharmD, BCPS4, Anish Patel, DO2
1Brooke Army Medical Center, San Antonio, TX; 2Brooke Army Medical Center, Fort Sam Houston, TX; 3AbbVie, Inc., Mettawa, IL; 4AbbVie, Inc., North Chicago, IL
Introduction: Crohn’s disease (CD) is characterized by transmural inflammation and ongoing inflammatory activity, which over time results in the accumulation of bowel damage, which may lead to complications such as strictures, fistulas/fissures, and abscesses, as well as disability. Optimally controlling inflammation early in the disease course of CD, during the ‘window of opportunity,’ may be the best way to change disease course. Recent evidence and clinical practice guidelines suggest that early biologic therapy is preferred in treating moderate to severe CD. Early use of biologic therapy and achievement of mucosal healing can contribute to disease course modification. We hypothesize that significantly more CD patients treated within 2 years of diagnosis will achieve clinical remission and have less CD-related complications than those treated 2 or more years after diagnosis.
Methods: We conducted a retrospective cohort study of CD patients treated within the Military Health System to assess the relationship of timing of initiation of biologic therapy with the control of CD. Data was collected from January 1, 2013 to December 30, 2020 to measure the course of patients’ disease as determined by clinical, biochemical, radiologic, and endoscopic/histologic findings, with an assessment of clinical outcomes and complications to include CD-related emergency room visits, steroid use, hospitalizations, and surgeries.
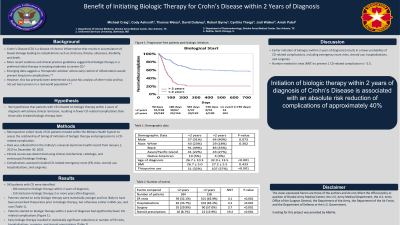
Results: 343 patients with CD were identified, of which 184 were started on biologic therapy within 2 years of diagnosis, while 159 were started on biologic therapy 2 or more years after diagnosis. Patients who initiated biologic therapy within 2 years of diagnosis had significantly fewer CD-related complications (p< 0.0001) (Image 1a). Evidence of perianal disease at diagnosis was predictive of an increased likelihood of CD-related complications (Image 1b). Patients on monotherapy with thiopurines prior to biologic therapy were also more likely to experience CD-related complications (Image 1c).
Discussion: These findings demonstrate that earlier initiation of biologics (within 2 years of diagnosis) results in a lower probability of CD-related complications, including emergency room visits, steroid use, hospitalizations, and surgeries. This real-world study is one of the first to confirm prior clinical trial data on decreased complications in early initiation of biologic therapy in CD patients.

Disclosures:
Michael Craig, MD1, Cody Ashcroft, MD2, David Dulaney, MD2, Robert Byrne, MD2, Thomas Weiss, MD2, Cindy Theigs, RPH3, Jodi H. Walker, BS, PharmD, BCPS4, Anish Patel, DO2. B0362 - Impact of Early Biologic Therapy in Real-World Cohort of Crohn’s Disease Patients, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Brooke Army Medical Center, San Antonio, TX; 2Brooke Army Medical Center, Fort Sam Houston, TX; 3AbbVie, Inc., Mettawa, IL; 4AbbVie, Inc., North Chicago, IL
Introduction: Crohn’s disease (CD) is characterized by transmural inflammation and ongoing inflammatory activity, which over time results in the accumulation of bowel damage, which may lead to complications such as strictures, fistulas/fissures, and abscesses, as well as disability. Optimally controlling inflammation early in the disease course of CD, during the ‘window of opportunity,’ may be the best way to change disease course. Recent evidence and clinical practice guidelines suggest that early biologic therapy is preferred in treating moderate to severe CD. Early use of biologic therapy and achievement of mucosal healing can contribute to disease course modification. We hypothesize that significantly more CD patients treated within 2 years of diagnosis will achieve clinical remission and have less CD-related complications than those treated 2 or more years after diagnosis.
Methods: We conducted a retrospective cohort study of CD patients treated within the Military Health System to assess the relationship of timing of initiation of biologic therapy with the control of CD. Data was collected from January 1, 2013 to December 30, 2020 to measure the course of patients’ disease as determined by clinical, biochemical, radiologic, and endoscopic/histologic findings, with an assessment of clinical outcomes and complications to include CD-related emergency room visits, steroid use, hospitalizations, and surgeries.
Results: 343 patients with CD were identified, of which 184 were started on biologic therapy within 2 years of diagnosis, while 159 were started on biologic therapy 2 or more years after diagnosis. Patients who initiated biologic therapy within 2 years of diagnosis had significantly fewer CD-related complications (p< 0.0001) (Image 1a). Evidence of perianal disease at diagnosis was predictive of an increased likelihood of CD-related complications (Image 1b). Patients on monotherapy with thiopurines prior to biologic therapy were also more likely to experience CD-related complications (Image 1c).
Discussion: These findings demonstrate that earlier initiation of biologics (within 2 years of diagnosis) results in a lower probability of CD-related complications, including emergency room visits, steroid use, hospitalizations, and surgeries. This real-world study is one of the first to confirm prior clinical trial data on decreased complications in early initiation of biologic therapy in CD patients.

Figure: Survival curves for complications with respect to timing of biologic start (1a), presence of perianal disease (1b) and thiopurine therapy prior to biologic stat (1c).
Disclosures:
Michael Craig indicated no relevant financial relationships.
Cody Ashcroft indicated no relevant financial relationships.
David Dulaney indicated no relevant financial relationships.
Robert Byrne indicated no relevant financial relationships.
Thomas Weiss indicated no relevant financial relationships.
Cindy Theigs: Abbvie – Employee, Stock Options.
Jodi Walker: Abbvie – Employee, Stock Options.
Anish Patel indicated no relevant financial relationships.
Michael Craig, MD1, Cody Ashcroft, MD2, David Dulaney, MD2, Robert Byrne, MD2, Thomas Weiss, MD2, Cindy Theigs, RPH3, Jodi H. Walker, BS, PharmD, BCPS4, Anish Patel, DO2. B0362 - Impact of Early Biologic Therapy in Real-World Cohort of Crohn’s Disease Patients, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

