Poster Session B - Monday Morning
Category: IBD
B0417 - Efficacy and Safety of Upadacitinib Maintenance Therapy in Patients With Moderately to Severely Active Ulcerative Colitis: Final Results From the Phase 3 U-ACHIEVE Maintenance Study
- WZ
Wen Zhou, MD, PhD
AbbVie Inc.
North Chicago, IL
Presenting Author(s)
1University Hospitals Leuven, Leuven, Brussels Hoofdstedelijk Gewest, Belgium; 2IRCCS Ospedale San Raffaele and University Vita-Salute San Raffaele, Milan, Molise, Italy; 3AbbVie Inc., North Chicago, IL; 4AbbVie, Inc., North Chicago, IL; 5CHU de Nice, Université Côte d’Azur, Nice, Provence-Alpes-Cote d'Azur, France; 6The Royal London Hospital, Barts Health NHS Trust, London, England, United Kingdom; 7University of Michigan, Ann Arbor, MI; 8Icahn School of Medicine at Mount Sinai, New York, NY; 9University of Calgary, Calgary, AB, Canada
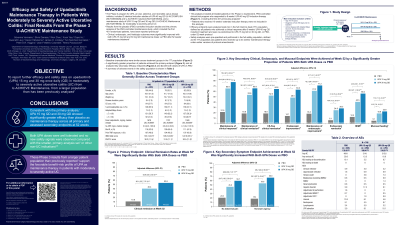
Introduction: Upadacitinib(UPA), has shown superior efficacy to placebo(PBO) in patients with moderate to severe active ulcerative colitis(UC) in two Phase 3 induction studies .1,2 Patients demonstrating clinical response per Adapted Mayo score with UPA 45mg once daily(QD) after 8 weeks(wks) induction were enrolled to U-ACHIEVE Maintenance.
Methods: U-ACHIEVE Maintenance efficacy data from the intent-to-treat(ITT) population, defined as UPA 45mg QD 8wk induction responders enrolled per protocol for 52wk maintenance, and safety data from the safety population, defined as patients who received ≥1 dose of study therapy(ITT plus patients receiving up to 44wksmaintenanceper prior versions of protocol amendments).
Results: In ITT population, 681 patients achieving clinical response after 8wks of induction were re-randomized to UPA 15mg(UPA15; n=225), UPA 30mg (UPA30; n=233), or PBO(n=223) maintenance. A greater proportion of patients achieved primary endpoint of clinical remission at Wk 52 with UPA15(40.4%) and UPA30(53.6%) vs PBO(10.8%; both p< 0.001), and secondary endpoints including endoscopic improvement and remission, maintenance of clinical remission, steroid-free clinical remission, and histologic-endoscopic mucosal improvement(all p< 0.001; Table). Safety evaluation included 746 patients(UPA15, n=250; UPA30, n=251; PBO, n=245). Of these, 8.4% experienced a serious adverse event(AE) with UPA15, 8.4% UPA30, and 9.4% PBO; 4.0%, 7.2%, and 10.2% experienced AEs leading to treatment discontinuation, respectively. The most common AEs were worsening UC with UPA15(11.6%) and PBO(30.2%), and nasopharyngitis with UPA30(10.4%). There were no deaths. Serious infections were reported in 3.6% of UPA15 patients, 2.8% UPA30, and 3.3% PBO. Herpes zoster was reported only with UPA(UPA15, 4.8%; UPA30, 5.6%). Malignancies excluding non-melanoma skin cancer were reported by one patient with PBO and UPA15, and two with UPA30. Major adverse cardiovascular events were reported in one PBO patient and one UPA30(n=0, UPA15), and venous thromboembolic events were reported in two patients each with UPA15 and UPA30(n=0, PBO).
Discussion: In UC patients who responded to induction therapy, both UPA15 and UPA30 were significantly more efficacious vs PBO as maintenance across primary and secondary endpoints. UPA doses were well tolerated, and there were no new safety signals with a larger population than previously reported.3 These results are consistent with previously published data.3
Primary and key secondary endpoints at Week 52 | PBO, n (%) [N]
N=223 | UPA 15 mg QD, n (%) [N] N=225 | Adjusted difference vs PBO, % (95% CI)a | UPA 30 mg QD, n (%) [N] N=233 | Adjusted difference vs PBO, % (95% CI)a |
Primary endpoint: Clinical remissionb | 24 (10.8) | 91 (40.4) | 30.1*** (22.7, 37.4) | 125 (53.6) | 42.9*** (35.4, 50.4) |
Maintenance of clinical responsec | 44 (21.5) [N=204] | 129 (65.6) [N=197] | 43.9*** (35.4, 52.5) | 168 (77.5) [N=217] | 55.6*** (47.8, 63.4) |
Endoscopic improvementd | 31 (14.1) | 109 (48.5) | 34.4*** (26.7, 42.1) | 147 (63.3) | 49.0*** (41.4, 56.7) |
Maintenance of clinical remissione | 16 (18.8) [N=85] | 41 (53.6) [N=76] | 34.9*** (21.2, 48.5) | 57 (65.8) [N=87] | 46.9*** (34.0, 59.8) |
Corticosteroid-free clinical remissionf | 16 (18.8) [N=85] | 40 (52.3) [N=76] | 33.7*** (20.0, 47.3) | 56 (64.6) [N=87] | 45.5*** (32.6, 58.5) |
Maintenance of endoscopic improvementg | 21 (18.4) [N=115] | 59 (61.2) [N=97] | 42.2*** (30.4, 53.9) | 84 (71.0) [N=118] | 51.5*** (40.9, 62.1) |
Endoscopic remissionh | 14 (6.1) | 56 (24.9) | 18.6*** (12.2, 25.0) | 66 (28.3) | 21.9*** (15.4, 28.5) |
Histologic-endoscopic mucosal improvementi
Mucosal healingj
| 27 (12.3)
11 (5.1)
| 91 (40.5)
42 (18.8)
| 28.5*** (21.1, 35.9)
13.5*** (7.8, 19.3) | 131 (56.0)
53 (22.6)
| 43.8*** (36.1, 51.5)
17.2*** (11.2, 23,3) |
***p< 0.001. The efficacy analysis was performed in patients who received up to 52 weeks’ maintenance treatment (ITT population). Non-responder imputation incorporating multiple imputations to handle missing data due to COVID-19 was used. aBased on adjusted Cochran–Mantel–Haenszel test adjusted for strata (corticosteroid use at Week 0 (yes or no), clinical remission status at Week 0 (yes or no), biologic-IR status at baseline (biologic-IR or non-biologic-IR)). bPer Adapted Mayo score ≤2: stool frequency subscore ≤1 and not greater than induction baseline, RBS=0, and ES ≤1. cMaintenance of clinical response, defined as a decrease in Adapted Mayo score ≥2 and ≥30% from induction baseline, plus a decrease in RBS ≥1 or an absolute RBS ≤1, at Week 52 among patients who achieved clinical response at the end of the induction therapy. dES ≤1. eMaintenance of CR at Week 52 among patients with CR at the end of the induction therapy. fCR at Week 52 and corticosteroid-free for ≥90 days prior to Week 52 among patients with CR at the end of the induction therapy. gEndoscopic improvement at Week 52 among patients with endoscopic improvement at the end of the induction therapy. hES=0. iES ≤1 and Geboes score ≤3.1. jES=0 and Geboes score < 2.0. CI, confidence interval; CR, clinical remission; ES, endoscopic subscore; IR, inadequate responders; ITT, intent-to-treat; PBO, placebo; QD, once daily; RBS, rectal bleeding subscore; UPA, upadacitinib |
|
|
|
|
|
Disclosures:
Séverine Vermeire, MD, PhD1, Silvio Danese, MD, PhD2, Wen Zhou, MD, PhD3, Xuan Yao, PhD4, Dapo Ilo, MBBS, MRCS, MSc4, John Liu, MD, MS4, Xavier Hébuterne, MD5, James Lindsay, DO6, Yuri Sanchez-Gonzalez, PhD4, Peter D. Higgins, MD, PhD, MSc7, Jean-Frederic Colombel, MD8, Remo Panaccione, MD9. B0417 - Efficacy and Safety of Upadacitinib Maintenance Therapy in Patients With Moderately to Severely Active Ulcerative Colitis: Final Results From the Phase 3 U-ACHIEVE Maintenance Study, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
