Back

Poster Session A - Sunday Afternoon
Category: Liver
A0562 - A Rare Case of Primary Biliary Cholangitis and Hepatic Sarcoidosis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Annie Shergill, MD
Larkin Community Hospital
Fresno, CA
Presenting Author(s)
Annie Shergill, MD1, Abhishek Gulati, MD2
1Larkin Community Hospital, Fresno, CA; 2Clovis Community Medical Center, Clovis, CA
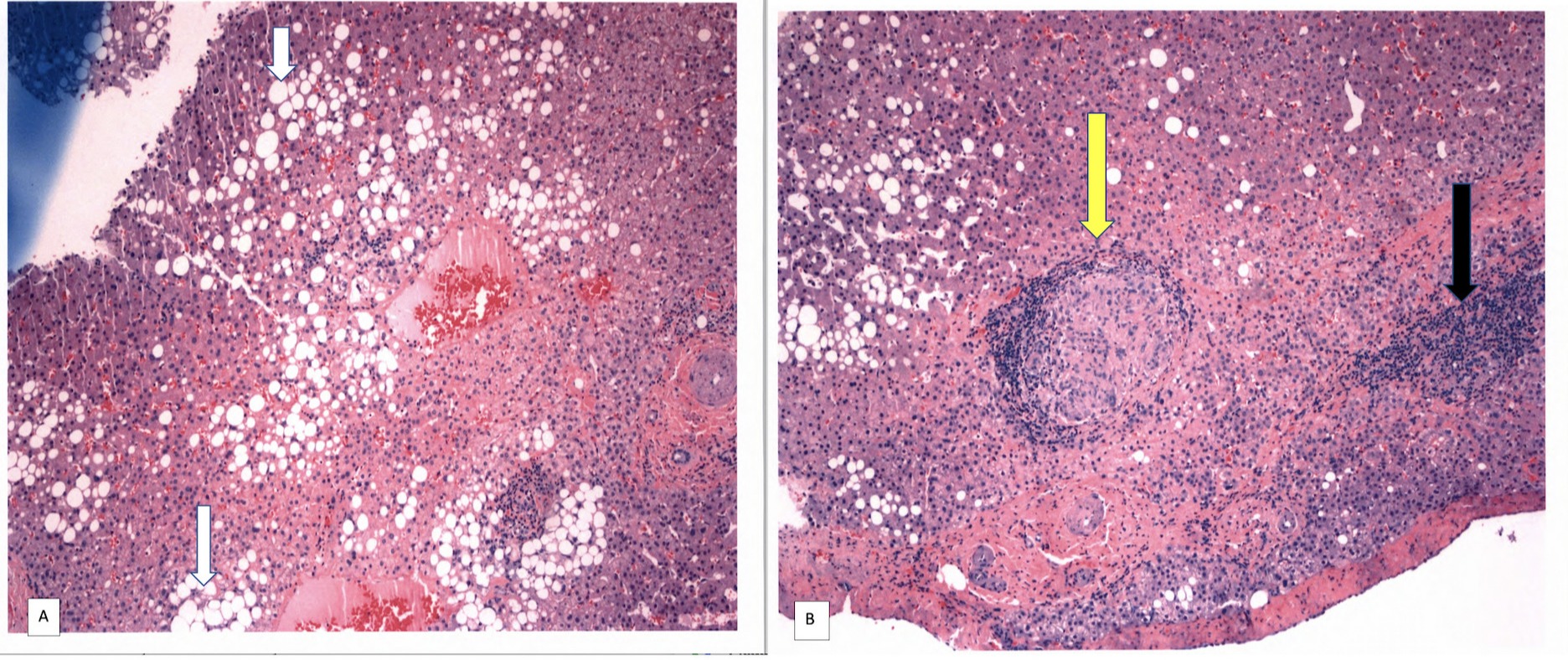
Introduction: Primary biliary cholangitis (PBC) is a disease characterized by immune-mediated destruction of intrahepatic bile ducts resulting in cholestatic liver disease. Sarcoidosis is a multisystem, chronic granulomatous disease of unknown etiology with hepatic involvement seen in majority of the patients. Very rarely, hepatic sarcoidosis can present as diffuse intrahepatic biliary inflammation, destruction and cholestatic liver disease, thereby resembling PBC. We present a rare case of hepatic sarcoidosis with PBC and non-alcoholic fatty liver disease (NAFLD).
Case Description/Methods: A 47 year old female with history of asymptomatic pulmonary sarcoidosis, type 2 diabetes mellitus, morbid obesity underwent liver biopsy for evaluation of fatty liver and abnormal liver enzymes (AST 41 U/L, ALT 55 U/L, alkaline phosphatase 238 U/L, Total bilirubin 0.5 mg/dL). Biopsy showed steatohepatitis with non-necrotizing granulomas consistent with sarcoidosis. Patient was asymptomatic and not on treatment for sarcoidosis or any other hepatotoxic medications. Social history was pertinent for no significant alcohol intake. Patient continued to have persistently abnormal liver enzymes and was further evaluated with a comprehensive chronic liver disease work up. This came back positive for Anti-mitochondrial antibody (AMA), raising suspicion for underlying PBC. Patient underwent repeat liver biopsy which showed similar findings of steatohepatitis and non-necrotizing granulomas along with focally identified biliary inflammation suggestive of underlying chronic biliary disease such as PBC given positive serologic testing for AMA. Iron and copper stains were negative. Patient was subsequently started on therapy with Ursodiol.
Discussion: Hepatic sarcoidosis most commonly manifests as non-necrotizing granulomas as seen on liver biopsy. However, in this case the liver biopsy showed evidence of three pathological processes- PBC, sarcoidosis and NAFLD. Patients with hepatic sarcoidosis very rarely develop an underlying co-existing cholestatic liver disease. The postulated underlying mechanism of chronic cholestasis in sarcoidosis involves confluent granulomas causing granulomatous cholangitis and ductopenia. It is prudent to identify this co-existing pathological process in order to initiate appropriate treatment and prevent further hepatic damage. Therefore, chronic cholestasis in hepatic sarcoidosis should prompt extensive evaluation for an alternative cause of chronic liver disease.
Disclosures:
Annie Shergill, MD1, Abhishek Gulati, MD2. A0562 - A Rare Case of Primary Biliary Cholangitis and Hepatic Sarcoidosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Larkin Community Hospital, Fresno, CA; 2Clovis Community Medical Center, Clovis, CA
Introduction: Primary biliary cholangitis (PBC) is a disease characterized by immune-mediated destruction of intrahepatic bile ducts resulting in cholestatic liver disease. Sarcoidosis is a multisystem, chronic granulomatous disease of unknown etiology with hepatic involvement seen in majority of the patients. Very rarely, hepatic sarcoidosis can present as diffuse intrahepatic biliary inflammation, destruction and cholestatic liver disease, thereby resembling PBC. We present a rare case of hepatic sarcoidosis with PBC and non-alcoholic fatty liver disease (NAFLD).
Case Description/Methods: A 47 year old female with history of asymptomatic pulmonary sarcoidosis, type 2 diabetes mellitus, morbid obesity underwent liver biopsy for evaluation of fatty liver and abnormal liver enzymes (AST 41 U/L, ALT 55 U/L, alkaline phosphatase 238 U/L, Total bilirubin 0.5 mg/dL). Biopsy showed steatohepatitis with non-necrotizing granulomas consistent with sarcoidosis. Patient was asymptomatic and not on treatment for sarcoidosis or any other hepatotoxic medications. Social history was pertinent for no significant alcohol intake. Patient continued to have persistently abnormal liver enzymes and was further evaluated with a comprehensive chronic liver disease work up. This came back positive for Anti-mitochondrial antibody (AMA), raising suspicion for underlying PBC. Patient underwent repeat liver biopsy which showed similar findings of steatohepatitis and non-necrotizing granulomas along with focally identified biliary inflammation suggestive of underlying chronic biliary disease such as PBC given positive serologic testing for AMA. Iron and copper stains were negative. Patient was subsequently started on therapy with Ursodiol.
Discussion: Hepatic sarcoidosis most commonly manifests as non-necrotizing granulomas as seen on liver biopsy. However, in this case the liver biopsy showed evidence of three pathological processes- PBC, sarcoidosis and NAFLD. Patients with hepatic sarcoidosis very rarely develop an underlying co-existing cholestatic liver disease. The postulated underlying mechanism of chronic cholestasis in sarcoidosis involves confluent granulomas causing granulomatous cholangitis and ductopenia. It is prudent to identify this co-existing pathological process in order to initiate appropriate treatment and prevent further hepatic damage. Therefore, chronic cholestasis in hepatic sarcoidosis should prompt extensive evaluation for an alternative cause of chronic liver disease.
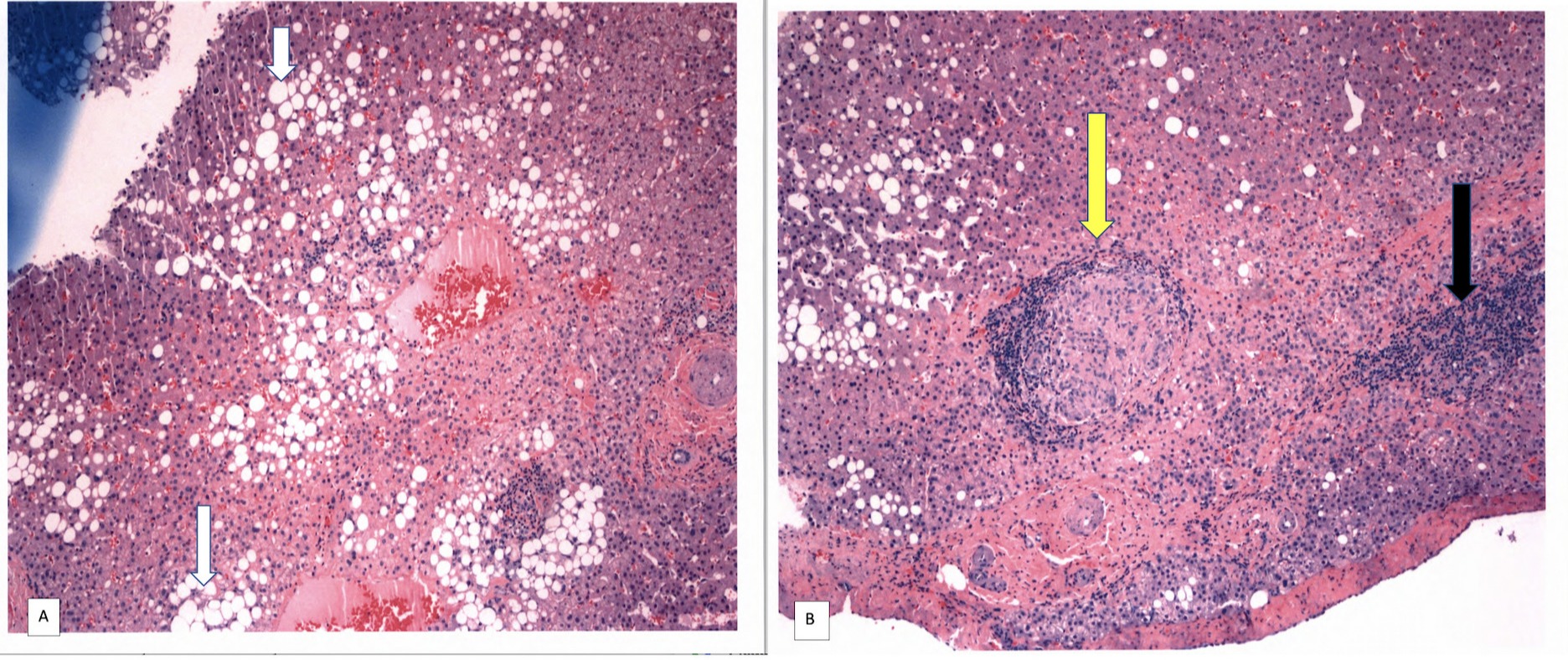
Figure: Figure 1A: Moderate large-droplet steatosis (white arrow) with mild to moderate lobular inflammation is seen.
Figure 1B: Scattered non-necrotizing granulomas (yellow arrow) with focal portal inflammation (black arrow) is seen.
Figure 1B: Scattered non-necrotizing granulomas (yellow arrow) with focal portal inflammation (black arrow) is seen.
Disclosures:
Annie Shergill indicated no relevant financial relationships.
Abhishek Gulati indicated no relevant financial relationships.
Annie Shergill, MD1, Abhishek Gulati, MD2. A0562 - A Rare Case of Primary Biliary Cholangitis and Hepatic Sarcoidosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
