Back

Poster Session B - Monday Morning
Category: Liver
B0500 - Gaps in Confirmatory Fibrosis Risk Assessment in Primary Care Patients With Nonalcoholic Fatty Liver Disease
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Joseph A. Moore, MD
Medical University of South Carolina
Charleston, SC
Presenting Author(s)
Joseph A. Moore, MD, Jingwen Zhang, MS, Andrew D. Schreiner, MD
Medical University of South Carolina, Charleston, SC
Introduction: As non-invasive fibrosis risk assessment strategies for nonalcoholic fatty liver disease (NAFLD) emerge, it is not known how often they are performed in primary care. We investigated the use of vibration-controlled elastography (VCTE) for fibrosis risk assessment in primary care patients with NAFLD and indeterminate-risk or greater serologic fibrosis risk assessments.
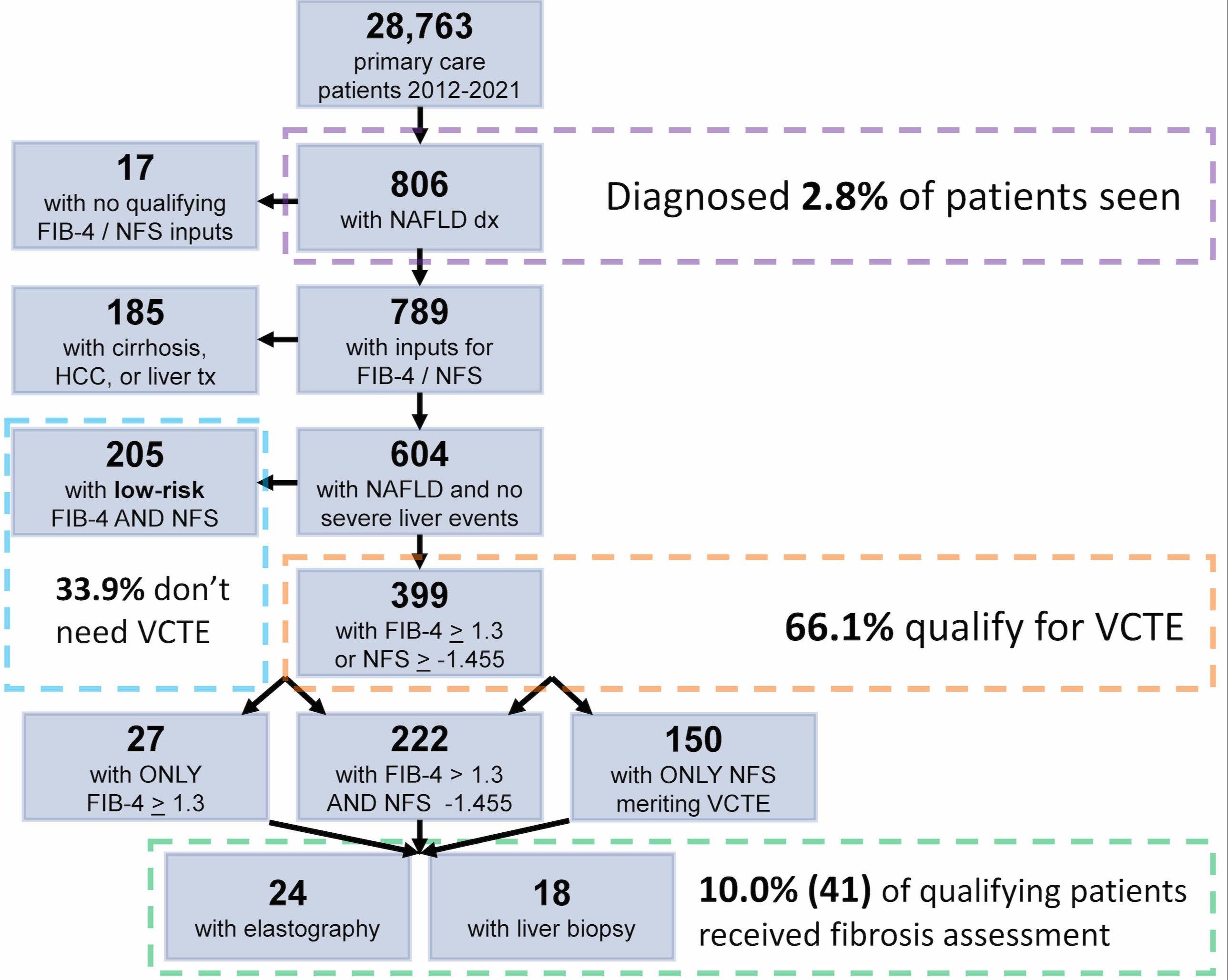
Methods: This retrospective cohort study of electronic health record data from a patient-centered medical home identified primary care patients with ICD-9/10 diagnoses of NAFLD from 2012 through 2021. Patients with a NAFLD diagnosis and qualifying inputs for Fibrosis-4 Index (FIB-4) and NAFLD Fibrosis Score (NFS) calculation within 3 years from the end of the study period were included. FIB-4 and NFS calculations required aminotransferase (aspartate [AST] and alanine [ALT]) results < 350 IU/L and platelet counts within 6 months of the AST and ALT values. Patients with a diagnosis of a severe liver outcome during the study period were excluded. The most recent FIB-4 and NFS scores were calculated and categorized by fibrosis risk. Charts were reviewed to identify the outcome of a confirmatory fibrosis risk assessment by liver elastography or liver biopsy any time during the study period for all patients with indeterminate-risk or higher FIB-4 ( >1.3) and NFS ( >-1.455) scores. Statistical analyses were performed using SAS version 9.4 (Cary, NC).
Results: The study sample included 604 patients with a diagnosis of NAFLD, inputs for serologic fibrosis risk score calculation, and no prior severe liver outcomes (Figure 1). Included patients were 60% female, 30% Black, had a mean age of 57 years, and a mean BMI of 32.2 m2/kg. Of the cohort, 45% had diabetes, 69% had hyperlipidemia, and 26% had cardiovascular disease. Two-thirds of included patients (399) had a FIB-4 or NFS score greater than low-risk, 19% (113) had a high-risk FIB-4 ( > 2.67) or NFS ( > 0.676) score, and 7% (44) had high-risk FIB-4 and NFS values. Of these 399 patients with an indication for a confirmatory fibrosis test, 10% (41) underwent VCTE (24) or liver biopsy (18) or both (1).
Discussion: Advanced fibrosis is a key indicator of future poor health outcomes in patients with NAFLD and a critical signal for primary care referral to hepatology. Even though much work is needed to improve NAFLD diagnosis in primary care, opportunities currently exist to improve confirmatory fibrosis risk assessment in patients with NAFLD.
Disclosures:
Joseph A. Moore, MD, Jingwen Zhang, MS, Andrew D. Schreiner, MD. B0500 - Gaps in Confirmatory Fibrosis Risk Assessment in Primary Care Patients With Nonalcoholic Fatty Liver Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Medical University of South Carolina, Charleston, SC
Introduction: As non-invasive fibrosis risk assessment strategies for nonalcoholic fatty liver disease (NAFLD) emerge, it is not known how often they are performed in primary care. We investigated the use of vibration-controlled elastography (VCTE) for fibrosis risk assessment in primary care patients with NAFLD and indeterminate-risk or greater serologic fibrosis risk assessments.
Methods: This retrospective cohort study of electronic health record data from a patient-centered medical home identified primary care patients with ICD-9/10 diagnoses of NAFLD from 2012 through 2021. Patients with a NAFLD diagnosis and qualifying inputs for Fibrosis-4 Index (FIB-4) and NAFLD Fibrosis Score (NFS) calculation within 3 years from the end of the study period were included. FIB-4 and NFS calculations required aminotransferase (aspartate [AST] and alanine [ALT]) results < 350 IU/L and platelet counts within 6 months of the AST and ALT values. Patients with a diagnosis of a severe liver outcome during the study period were excluded. The most recent FIB-4 and NFS scores were calculated and categorized by fibrosis risk. Charts were reviewed to identify the outcome of a confirmatory fibrosis risk assessment by liver elastography or liver biopsy any time during the study period for all patients with indeterminate-risk or higher FIB-4 ( >1.3) and NFS ( >-1.455) scores. Statistical analyses were performed using SAS version 9.4 (Cary, NC).
Results: The study sample included 604 patients with a diagnosis of NAFLD, inputs for serologic fibrosis risk score calculation, and no prior severe liver outcomes (Figure 1). Included patients were 60% female, 30% Black, had a mean age of 57 years, and a mean BMI of 32.2 m2/kg. Of the cohort, 45% had diabetes, 69% had hyperlipidemia, and 26% had cardiovascular disease. Two-thirds of included patients (399) had a FIB-4 or NFS score greater than low-risk, 19% (113) had a high-risk FIB-4 ( > 2.67) or NFS ( > 0.676) score, and 7% (44) had high-risk FIB-4 and NFS values. Of these 399 patients with an indication for a confirmatory fibrosis test, 10% (41) underwent VCTE (24) or liver biopsy (18) or both (1).
Discussion: Advanced fibrosis is a key indicator of future poor health outcomes in patients with NAFLD and a critical signal for primary care referral to hepatology. Even though much work is needed to improve NAFLD diagnosis in primary care, opportunities currently exist to improve confirmatory fibrosis risk assessment in patients with NAFLD.
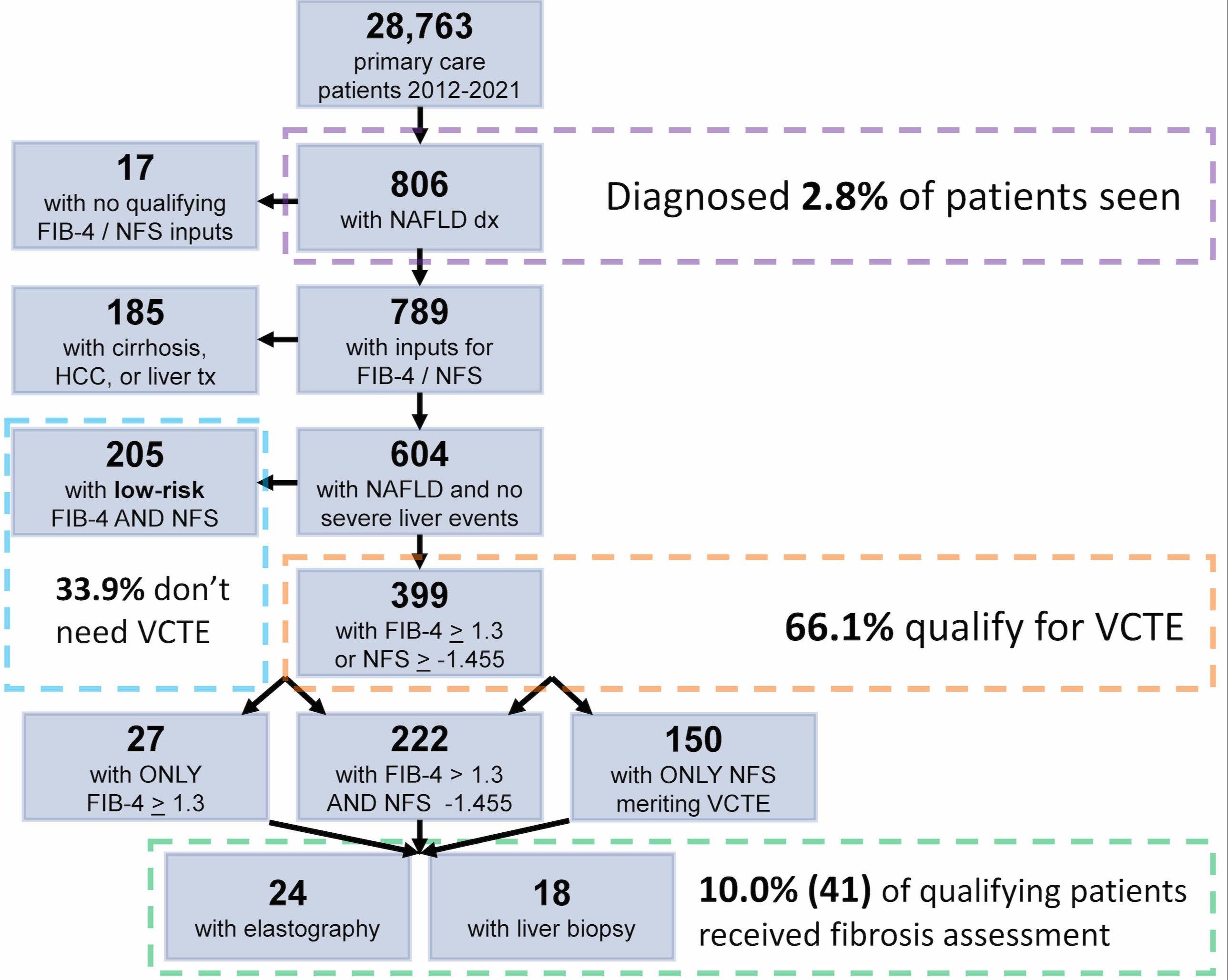
Figure: Figure 1. Study population with serologic fibrosis risk scores and confirmatory fibrosis assessment.
dx=diagnosis; HCC=hepatocellular carcinoma; tx= transplant
dx=diagnosis; HCC=hepatocellular carcinoma; tx= transplant
Disclosures:
Joseph Moore indicated no relevant financial relationships.
Jingwen Zhang indicated no relevant financial relationships.
Andrew Schreiner indicated no relevant financial relationships.
Joseph A. Moore, MD, Jingwen Zhang, MS, Andrew D. Schreiner, MD. B0500 - Gaps in Confirmatory Fibrosis Risk Assessment in Primary Care Patients With Nonalcoholic Fatty Liver Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
