Back

Poster Session B - Monday Morning
Category: Liver
B0577 - Hepatic Abscesses and Portal Vein Thrombosis Due to Fusobacterium Nucleatum Septicemia: Lemierre Syndrome Variant
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Fouad S. Jaber, MD
University of Missouri-Kansas City
KANSAS CITY, MO
Presenting Author(s)
Fouad S. Jaber, MD, Islam Mohamed, MD, Rawan Rajab, MD, Kaitlin Wittler, MD
University of Missouri-Kansas City, Kansas City, MO
Introduction: Fusobacterium species are well known to cause Lemierre syndrome. However, few cases had linked Fusobacterium nucleatum (F. nucleatum) to gastrointestinal (GI) variant of Lemierre syndrome. We report a rare case of Fusobacterium nucleatum septicemia with septic pylephlebitis and multiple liver abscesses, most likely from mild gastrointestinal primary infection.
Case Description/Methods: A 62-year-old female with a medical history of hypertension, and heart failure with reduced ejection fraction presented as a transfer from an outside hospital for evaluation of liver lesions. Patient presented with generalized malaise, confusion, low-grade fever, and body aches. One week prior to presentation, she had left-sided cramping abdominal pain associated with decreased appetite.
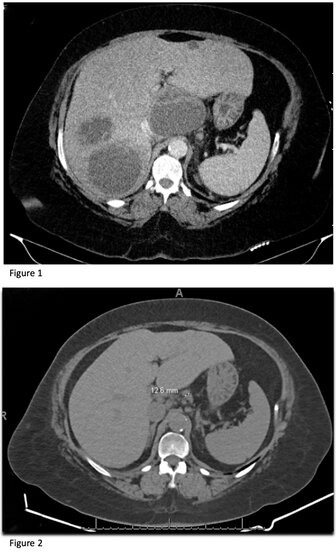
Labs on presentation were significant for leukocytosis, microcytic anemia with elevated ferritin, elevated alkaline phosphatase, and elevated creatinine. CT abdomen and pelvis with contrast (Figure 1) demonstrated numerous large hepatic lesions up to 9cm in size, subocclusive thrombus in the superior mesenteric and portal vein, several enlarged para-aortic lymph nodes, and chronic diverticulitis. Infectious work-up was significant for blood culture that grew fusobacterium nucleatum. Patient was started on enoxaparin and ampicillin-sulbactam. MRCP redemonstrated multiple predominantly cystic hepatic masses suspicious for abscess versus metastatic disease. CT chest and Brain MRI were unrevealing. Colonoscopy showed moderate, benign-appearing, 10cm stenosis in the distal sigmoid colon, and extensive diverticula. Tumor markers were negative. Echo was negative for vegetations.
Interventional radiology performed aspiration of the left large and right hepatic cysts and placed 2 drains which yielded purulent fluid with cytology showing degenerative cells, neutrophils, and negative for malignancy. Patient was switched to ertapenem outpatient and apixaban. Repeat CT abdomen/pelvis (Figure 2) showed a decrease in size of the multiple hepatic abscesses and mild residual non-occlusive thrombus. Hepatic drains were removed, and patient was switched to oral Augmentin.
Discussion: Our patient had portal vein thrombosis, splenic vein thrombosis and hepatic abscesses presumably from primary GI infection likely mild diverticulitis. This picture may mimic metastatic liver cancer with portal vein thrombosis. Exclusion of malignancy and distinguishing clinical features should be identified early to initiate antimicrobial therapy and anticoagulation.
Disclosures:
Fouad S. Jaber, MD, Islam Mohamed, MD, Rawan Rajab, MD, Kaitlin Wittler, MD. B0577 - Hepatic Abscesses and Portal Vein Thrombosis Due to Fusobacterium Nucleatum Septicemia: Lemierre Syndrome Variant, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Missouri-Kansas City, Kansas City, MO
Introduction: Fusobacterium species are well known to cause Lemierre syndrome. However, few cases had linked Fusobacterium nucleatum (F. nucleatum) to gastrointestinal (GI) variant of Lemierre syndrome. We report a rare case of Fusobacterium nucleatum septicemia with septic pylephlebitis and multiple liver abscesses, most likely from mild gastrointestinal primary infection.
Case Description/Methods: A 62-year-old female with a medical history of hypertension, and heart failure with reduced ejection fraction presented as a transfer from an outside hospital for evaluation of liver lesions. Patient presented with generalized malaise, confusion, low-grade fever, and body aches. One week prior to presentation, she had left-sided cramping abdominal pain associated with decreased appetite.
Labs on presentation were significant for leukocytosis, microcytic anemia with elevated ferritin, elevated alkaline phosphatase, and elevated creatinine. CT abdomen and pelvis with contrast (Figure 1) demonstrated numerous large hepatic lesions up to 9cm in size, subocclusive thrombus in the superior mesenteric and portal vein, several enlarged para-aortic lymph nodes, and chronic diverticulitis. Infectious work-up was significant for blood culture that grew fusobacterium nucleatum. Patient was started on enoxaparin and ampicillin-sulbactam. MRCP redemonstrated multiple predominantly cystic hepatic masses suspicious for abscess versus metastatic disease. CT chest and Brain MRI were unrevealing. Colonoscopy showed moderate, benign-appearing, 10cm stenosis in the distal sigmoid colon, and extensive diverticula. Tumor markers were negative. Echo was negative for vegetations.
Interventional radiology performed aspiration of the left large and right hepatic cysts and placed 2 drains which yielded purulent fluid with cytology showing degenerative cells, neutrophils, and negative for malignancy. Patient was switched to ertapenem outpatient and apixaban. Repeat CT abdomen/pelvis (Figure 2) showed a decrease in size of the multiple hepatic abscesses and mild residual non-occlusive thrombus. Hepatic drains were removed, and patient was switched to oral Augmentin.
Discussion: Our patient had portal vein thrombosis, splenic vein thrombosis and hepatic abscesses presumably from primary GI infection likely mild diverticulitis. This picture may mimic metastatic liver cancer with portal vein thrombosis. Exclusion of malignancy and distinguishing clinical features should be identified early to initiate antimicrobial therapy and anticoagulation.
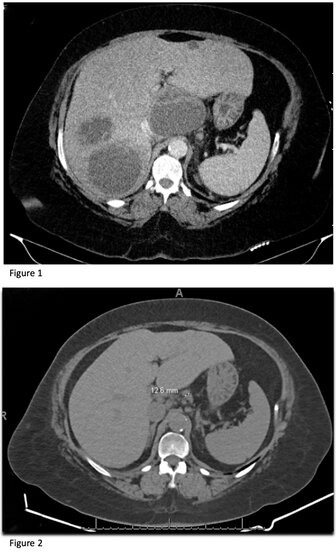
Figure: Figure 1: numerous large hepatic lesions up to 9 cm in size
Figure 2: significant decrease in size of multiple hepatic lesions
Figure 2: significant decrease in size of multiple hepatic lesions
Disclosures:
Fouad Jaber indicated no relevant financial relationships.
Islam Mohamed indicated no relevant financial relationships.
Rawan Rajab indicated no relevant financial relationships.
Kaitlin Wittler indicated no relevant financial relationships.
Fouad S. Jaber, MD, Islam Mohamed, MD, Rawan Rajab, MD, Kaitlin Wittler, MD. B0577 - Hepatic Abscesses and Portal Vein Thrombosis Due to Fusobacterium Nucleatum Septicemia: Lemierre Syndrome Variant, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

