Back

Poster Session B - Monday Morning
Category: Small Intestine
B0670 - A Case of Invasive Gastrointestinal Mold Infection
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Boris Zhong, DO, MS
Baylor Scott & White
Temple, TX
Presenting Author(s)
Award: Presidential Poster Award
Tyson Amundsen, MD1, Boris Zhong, DO, MS2, James Risinger, BS3, Mario A. Martinez, MD, MS4, Hector Ramirez, MD2
1University of Tennessee Health Science Center, Bartlett, TN; 2Baylor Scott & White, Temple, TX; 3Texas A&M School of Medicine, Temple, TX; 4Baylor Scott and White Health, Temple, TX
Introduction: Invasive mold infections can be devastating and are mostly seen in patients with hematologic malignancies, profound neutropenia, solid organ or hematopoietic cell transplantation, and poorly controlled diabetes mellitus. Mucormycosis is caused by a group of ubiquitous molds called Mucormycetes and characterized by tissue infarction and necrosis that results from invasion of the vasculature by hyphae. We present a rare case of a patient with invasive gastrointestinal mold infection.
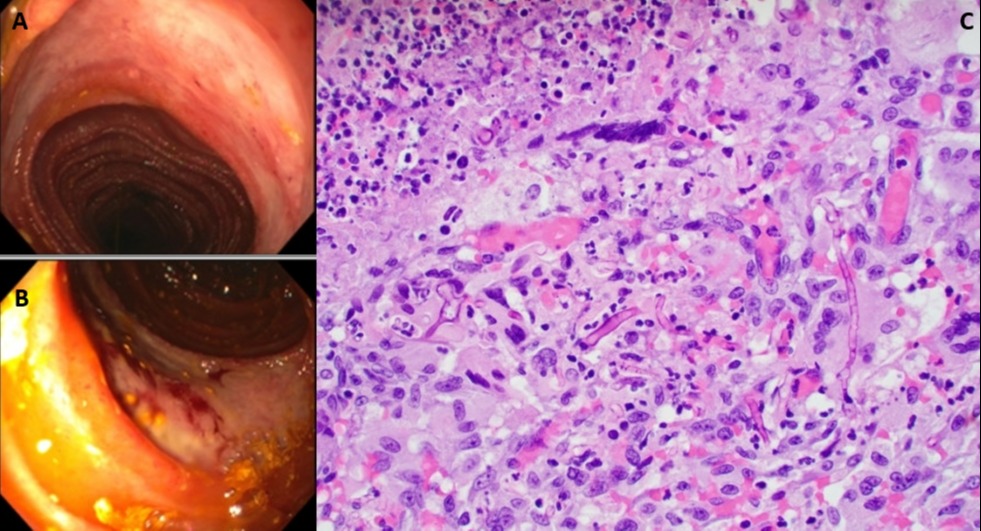
Case Description/Methods: A 40-year-old male with chronic inflammatory demyelinating polyneuropathy (CIDP) was admitted for autologous stem cell transplantation (ASCT). Initial hospitalization was complicated by neutropenic fever and C. difficile enteritis treated with Fidaxomicin. He was admitted one month later for nausea, vomiting and push enteroscopy revealed two circumferential deep small bowel ulcerations and a jejunal stricture too distal to be reached. Ulcer biopsies showed granulation tissue and was positive for Cytomegalovirus. He was treated with Valganciclovir and initiated on TPN. One week later, he had a third admission for intractable nausea and vomiting due to a small bowel obstruction. He failed conservative management and underwent diagnostic laparoscopy that revealed five strictures in the distal small bowel which were all resected with two small bowel resections and re-anastomosed. Histopathology of resected jejunum showed necrotizing granulomatous inflammation with aseptated fungal hyphae concerning for Mucormycosis, which was not identified on fungal PCR. He was treated with liposomal Amphotericin B then transitioned to oral Isavuconazole before making a full recovery.
Discussion: The most common presentation of Mucormycosis is a rhino-orbital-cerebral infection. Gastrointestinal infection is rare in living patients and has been estimated to occur in around 7% of all Mucormycosis cases and carries mortality as high as 85%. Our patient had a history of refractory CIDP and underwent chemotherapy for ASCT that was complicated by development of C. difficile and CMV gastrointestinal infections and small bowel obstruction necessitating endoscopic intervention which led to exploratory laparoscopy for surgical resection and the diagnosis of invasive Mucormycosis. Although invasive GI Mucormycosis is rare, in severely immunocompromised patients with unexplained gastrointestinal symptoms and multiple risk factors as presented in our patient, this infectious organism can be considered in the differential.
Disclosures:
Tyson Amundsen, MD1, Boris Zhong, DO, MS2, James Risinger, BS3, Mario A. Martinez, MD, MS4, Hector Ramirez, MD2. B0670 - A Case of Invasive Gastrointestinal Mold Infection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Tyson Amundsen, MD1, Boris Zhong, DO, MS2, James Risinger, BS3, Mario A. Martinez, MD, MS4, Hector Ramirez, MD2
1University of Tennessee Health Science Center, Bartlett, TN; 2Baylor Scott & White, Temple, TX; 3Texas A&M School of Medicine, Temple, TX; 4Baylor Scott and White Health, Temple, TX
Introduction: Invasive mold infections can be devastating and are mostly seen in patients with hematologic malignancies, profound neutropenia, solid organ or hematopoietic cell transplantation, and poorly controlled diabetes mellitus. Mucormycosis is caused by a group of ubiquitous molds called Mucormycetes and characterized by tissue infarction and necrosis that results from invasion of the vasculature by hyphae. We present a rare case of a patient with invasive gastrointestinal mold infection.
Case Description/Methods: A 40-year-old male with chronic inflammatory demyelinating polyneuropathy (CIDP) was admitted for autologous stem cell transplantation (ASCT). Initial hospitalization was complicated by neutropenic fever and C. difficile enteritis treated with Fidaxomicin. He was admitted one month later for nausea, vomiting and push enteroscopy revealed two circumferential deep small bowel ulcerations and a jejunal stricture too distal to be reached. Ulcer biopsies showed granulation tissue and was positive for Cytomegalovirus. He was treated with Valganciclovir and initiated on TPN. One week later, he had a third admission for intractable nausea and vomiting due to a small bowel obstruction. He failed conservative management and underwent diagnostic laparoscopy that revealed five strictures in the distal small bowel which were all resected with two small bowel resections and re-anastomosed. Histopathology of resected jejunum showed necrotizing granulomatous inflammation with aseptated fungal hyphae concerning for Mucormycosis, which was not identified on fungal PCR. He was treated with liposomal Amphotericin B then transitioned to oral Isavuconazole before making a full recovery.
Discussion: The most common presentation of Mucormycosis is a rhino-orbital-cerebral infection. Gastrointestinal infection is rare in living patients and has been estimated to occur in around 7% of all Mucormycosis cases and carries mortality as high as 85%. Our patient had a history of refractory CIDP and underwent chemotherapy for ASCT that was complicated by development of C. difficile and CMV gastrointestinal infections and small bowel obstruction necessitating endoscopic intervention which led to exploratory laparoscopy for surgical resection and the diagnosis of invasive Mucormycosis. Although invasive GI Mucormycosis is rare, in severely immunocompromised patients with unexplained gastrointestinal symptoms and multiple risk factors as presented in our patient, this infectious organism can be considered in the differential.
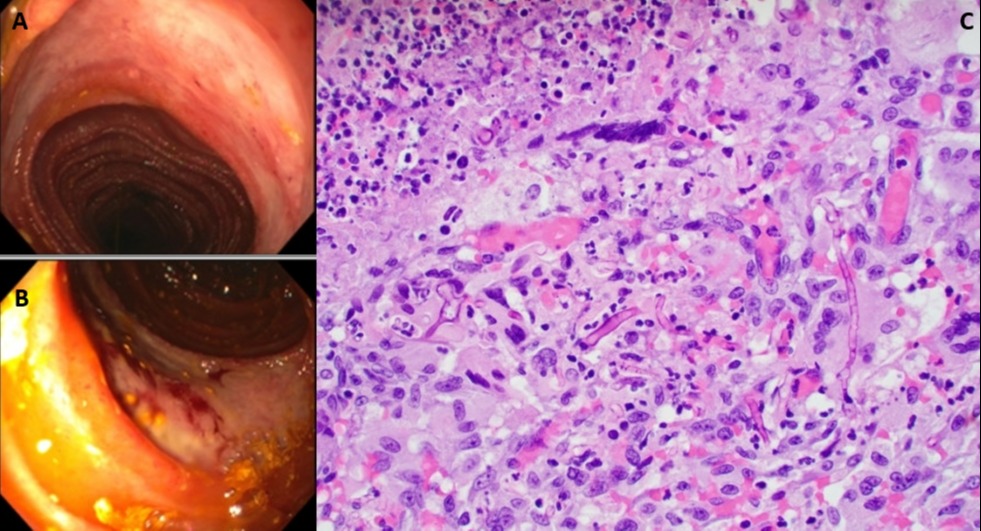
Figure: (A, B) Circumferential ulcerations seen in the small bowel on push enteroscopy. (C) Mucosal ulceration with underlying necrotizing granulomatous inflammation in the deep muscularis propria/pericolonic adipose tissue with non-septated fungal hyphae present.
Disclosures:
Tyson Amundsen indicated no relevant financial relationships.
Boris Zhong indicated no relevant financial relationships.
James Risinger indicated no relevant financial relationships.
Mario Martinez: Agenus – Stock-privately held company. Alphatec – Stock-privately held company. Catalyst Pharmaceuticals – Stock-privately held company. Clovis Oncology – Stock-privately held company. Moderna – Stock-privately held company. Opko Health – Stock-privately held company. Unity Biotechnology – Stock-privately held company. Zynerba – Stock-privately held company.
Hector Ramirez indicated no relevant financial relationships.
Tyson Amundsen, MD1, Boris Zhong, DO, MS2, James Risinger, BS3, Mario A. Martinez, MD, MS4, Hector Ramirez, MD2. B0670 - A Case of Invasive Gastrointestinal Mold Infection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

