Back

Poster Session B - Monday Morning
Category: Liver
B0542 - Hepatic Amyloidosis With Multi-Organ Involvement
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Robert J. Duve, MD, MA
University at Buffalo
Buffalo, NY
Presenting Author(s)
Robert J. Duve, MD, MA, Tiberiu Moga, MD, Kevin Yang, MD, Thomas C. Mahl, MD
University at Buffalo, Buffalo, NY
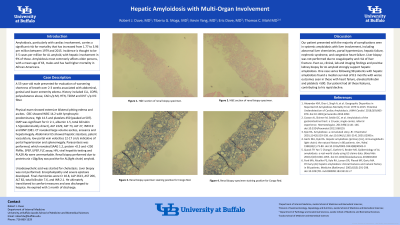
Introduction: Amyloidosis, particularly with cardiac involvement, carries a significant risk for mortality that has increased from 1.77 to 3.96 per million between 1979 and 2015. Incidence is thought to be 3-5 cases per million for AL amyloid, with hepatic involvement in 9% of those. Amyloidosis most commonly affects older persons, with a mean age of 63, males and has had higher mortality in African Americans.
Case Description/Methods: A 55-year-old male presented for evaluation of worsening shortness of breath over 2-3 weeks associated with abdominal, genital and lower extremity edema. History included CLL, COPD, polysubstance abuse, CAD s/p MI, HTN, T2DM and DVT s/p IVC filter.
Physical exam showed extensive bilateral pitting edema and ascites. CBC showed WBC 14.2 with lymphocytic predominance, Hgb 14.5 and platelets 450 (peaked at 507). CMP was significant for Cr 2.1, albumin 1.5, total bilirubin 1.5(predominantly direct), ALP 2229, AST 73, ALT 27, INR 0.9 and BNP 2381. CT revealed large volume ascites, anasarca and hepatomegaly. Abdominal US showed hepatic steatosis, patent vasculature, low portal vein velocities 12-17 cm/s indicative of portal hypertension and splenomegaly. Paracentesis was performed, which revealed SAAG 1.2, protein < 0.5 and < 250 PMNs. SPEP, UPEP, FLC assay, HIV, viral hepatitis testing and PLA2R Ab were unremarkable. Renal biopsy performed due to proteinuria >10g/day was positive for AL(light chain) amyloid.
Ursodeoxycholic acid was started for cholestasis. Liver biopsy was not performed. Encephalopathy and severe epistaxis developed. Final chemistries were Cr 10.8, ALP 2613, AST 206, ALT 82, total bilirubin 7.6, and INR 2.1. He ultimately transitioned to comfort measures and was discharged to hospice. He expired with 1 month of discharge.
Discussion: Our patient presented with the majority of complications seen in systemic amyloidosis with liver involvement, including abnormal liver chemistries, portal hypertension, hepatic failure, nephrotic syndrome, and congestive heart failure. Liver biopsy was not performed due to coagulopathy and risk of liver fracture. Even so, clinical, lab and imaging findings and positive kidney biopsy for Al amyloid strongly support hepatic amyloidosis. One case series following 98 patients with hepatic amyloidosis found a median survival of 8.5 months with worse outcomes seen in those with heart failure, elevated bilirubin and platelets >500. Our patient had all these features, contributing to his rapid decline.
Disclosures:
Robert J. Duve, MD, MA, Tiberiu Moga, MD, Kevin Yang, MD, Thomas C. Mahl, MD. B0542 - Hepatic Amyloidosis With Multi-Organ Involvement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University at Buffalo, Buffalo, NY
Introduction: Amyloidosis, particularly with cardiac involvement, carries a significant risk for mortality that has increased from 1.77 to 3.96 per million between 1979 and 2015. Incidence is thought to be 3-5 cases per million for AL amyloid, with hepatic involvement in 9% of those. Amyloidosis most commonly affects older persons, with a mean age of 63, males and has had higher mortality in African Americans.
Case Description/Methods: A 55-year-old male presented for evaluation of worsening shortness of breath over 2-3 weeks associated with abdominal, genital and lower extremity edema. History included CLL, COPD, polysubstance abuse, CAD s/p MI, HTN, T2DM and DVT s/p IVC filter.
Physical exam showed extensive bilateral pitting edema and ascites. CBC showed WBC 14.2 with lymphocytic predominance, Hgb 14.5 and platelets 450 (peaked at 507). CMP was significant for Cr 2.1, albumin 1.5, total bilirubin 1.5(predominantly direct), ALP 2229, AST 73, ALT 27, INR 0.9 and BNP 2381. CT revealed large volume ascites, anasarca and hepatomegaly. Abdominal US showed hepatic steatosis, patent vasculature, low portal vein velocities 12-17 cm/s indicative of portal hypertension and splenomegaly. Paracentesis was performed, which revealed SAAG 1.2, protein < 0.5 and < 250 PMNs. SPEP, UPEP, FLC assay, HIV, viral hepatitis testing and PLA2R Ab were unremarkable. Renal biopsy performed due to proteinuria >10g/day was positive for AL(light chain) amyloid.
Ursodeoxycholic acid was started for cholestasis. Liver biopsy was not performed. Encephalopathy and severe epistaxis developed. Final chemistries were Cr 10.8, ALP 2613, AST 206, ALT 82, total bilirubin 7.6, and INR 2.1. He ultimately transitioned to comfort measures and was discharged to hospice. He expired with 1 month of discharge.
Discussion: Our patient presented with the majority of complications seen in systemic amyloidosis with liver involvement, including abnormal liver chemistries, portal hypertension, hepatic failure, nephrotic syndrome, and congestive heart failure. Liver biopsy was not performed due to coagulopathy and risk of liver fracture. Even so, clinical, lab and imaging findings and positive kidney biopsy for Al amyloid strongly support hepatic amyloidosis. One case series following 98 patients with hepatic amyloidosis found a median survival of 8.5 months with worse outcomes seen in those with heart failure, elevated bilirubin and platelets >500. Our patient had all these features, contributing to his rapid decline.
Disclosures:
Robert Duve indicated no relevant financial relationships.
Tiberiu Moga indicated no relevant financial relationships.
Kevin Yang indicated no relevant financial relationships.
Thomas Mahl indicated no relevant financial relationships.
Robert J. Duve, MD, MA, Tiberiu Moga, MD, Kevin Yang, MD, Thomas C. Mahl, MD. B0542 - Hepatic Amyloidosis With Multi-Organ Involvement, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

