Back

Poster Session B - Monday Morning
Category: Small Intestine
B0659 - Small Bowel Enteropathy Induced by Immune Checkpoint Inhibitors: A Case Series
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Jessica El Halabi, MD, MBI
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Jessica El Halabi, MD, MBI, Natalie Farha, MD, Pauline Funchain, MD, Jessica Philpott, MD, PHD
Cleveland Clinic, Cleveland, OH
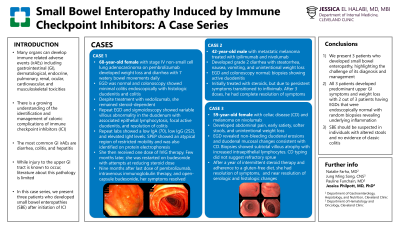
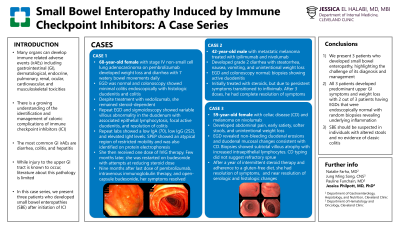
Introduction: While there is a growing understanding of the identification and management of colonic complications of immune checkpoint inhibitors (ICI), less is known about proximal intestinal complications. In this case series, we present 3 patients who developed small bowel enteropathies (SBE) after initiation of ICI.
Case Description/Methods: Case 1: A 68-year-old female with stage IV non-small cell lung adenocarcinoma on pembrolizumab developed diarrhea with 7 watery bowel movements daily. EGD was normal and colonoscopy showed minimal sigmoid erythema endoscopically with histologic duodenitis and colitis. Despite treatment with vedolizumab, she remained steroid-dependent. Repeat EGD and sigmoidoscopy showed variable villous abnormality in the duodenum with associated epithelial lymphocytosis, focal active duodenitis, and resolution of colitis. Serologic evaluation revealed hypogammagobulinemia. Nine months after last dose of pembrolizumab, and ultimately therapy with intravenous immunoglobulin therapy and open-capsule budesonide, her symptoms resolved.
Case 2: A 42-year-old male with metastatic melanoma treated with ipilimumab and nivolumab developed grade 2 diarrhea with steatorrhea, nausea, vomiting, and unintentional weight loss. EGD was endoscopically normal with biopsies showing active duodenitis with normal colonoscopy. He was initially treated with steroids, but due to persistent symptoms transitioned to infliximab. After receiving 3 doses of infliximab, he had complete resolution of symptoms.
Case 3: A 59-year-old female with celiac disease (CD) and metastatic melanoma was started on nivolumab. She developed abdominal pain, early satiety, softer stools, and unintentional weight loss. EGD revealed non-bleeding duodenal erosions and duodenal mucosal changes consistent with celiac disease. Biopsies showed subtotal villous atrophy with increased intraepithelial lymphocytes. CD typing did not suggest refractory sprue. Her presentation was suggestive of a nivolumab-induced exacerbation of CD. After a year of intermittent steroid therapy and adherence to a gluten-free diet, symptoms resolved. Repeat EGD with biopsies showed normal villi and reduced intraepithelial lymphocytes.
Discussion: In this case series, we present three patients who developed SBE, highlighting the challenge of its diagnosis and management. SBE should be suspected in individuals with altered stools and no evidence of classic colitis.
Disclosures:
Jessica El Halabi, MD, MBI, Natalie Farha, MD, Pauline Funchain, MD, Jessica Philpott, MD, PHD. B0659 - Small Bowel Enteropathy Induced by Immune Checkpoint Inhibitors: A Case Series, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Cleveland Clinic, Cleveland, OH
Introduction: While there is a growing understanding of the identification and management of colonic complications of immune checkpoint inhibitors (ICI), less is known about proximal intestinal complications. In this case series, we present 3 patients who developed small bowel enteropathies (SBE) after initiation of ICI.
Case Description/Methods: Case 1: A 68-year-old female with stage IV non-small cell lung adenocarcinoma on pembrolizumab developed diarrhea with 7 watery bowel movements daily. EGD was normal and colonoscopy showed minimal sigmoid erythema endoscopically with histologic duodenitis and colitis. Despite treatment with vedolizumab, she remained steroid-dependent. Repeat EGD and sigmoidoscopy showed variable villous abnormality in the duodenum with associated epithelial lymphocytosis, focal active duodenitis, and resolution of colitis. Serologic evaluation revealed hypogammagobulinemia. Nine months after last dose of pembrolizumab, and ultimately therapy with intravenous immunoglobulin therapy and open-capsule budesonide, her symptoms resolved.
Case 2: A 42-year-old male with metastatic melanoma treated with ipilimumab and nivolumab developed grade 2 diarrhea with steatorrhea, nausea, vomiting, and unintentional weight loss. EGD was endoscopically normal with biopsies showing active duodenitis with normal colonoscopy. He was initially treated with steroids, but due to persistent symptoms transitioned to infliximab. After receiving 3 doses of infliximab, he had complete resolution of symptoms.
Case 3: A 59-year-old female with celiac disease (CD) and metastatic melanoma was started on nivolumab. She developed abdominal pain, early satiety, softer stools, and unintentional weight loss. EGD revealed non-bleeding duodenal erosions and duodenal mucosal changes consistent with celiac disease. Biopsies showed subtotal villous atrophy with increased intraepithelial lymphocytes. CD typing did not suggest refractory sprue. Her presentation was suggestive of a nivolumab-induced exacerbation of CD. After a year of intermittent steroid therapy and adherence to a gluten-free diet, symptoms resolved. Repeat EGD with biopsies showed normal villi and reduced intraepithelial lymphocytes.
Discussion: In this case series, we present three patients who developed SBE, highlighting the challenge of its diagnosis and management. SBE should be suspected in individuals with altered stools and no evidence of classic colitis.
Disclosures:
Jessica El Halabi indicated no relevant financial relationships.
Natalie Farha indicated no relevant financial relationships.
Pauline Funchain: BMS – Grant/Research Support. Eisai – Consultant. GigaGen – Advisory Committee/Board Member. Novartis – Consultant. Pfizer – Grant/Research Support. Taiho Oncology – Grant/Research Support.
Jessica Philpott: Abbvie – Speakers Bureau.
Jessica El Halabi, MD, MBI, Natalie Farha, MD, Pauline Funchain, MD, Jessica Philpott, MD, PHD. B0659 - Small Bowel Enteropathy Induced by Immune Checkpoint Inhibitors: A Case Series, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
