Back

Poster Session C - Monday Afternoon
Category: Esophagus
C0205 - Fundoplication Alone and Class II Obesity or Higher Are Associated With the Need to Restart Proton Pump Inhibitors After Anti-Reflux Surgery in Patients With Hiatal Hernia
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Pedro Cortes, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Pedro Cortés, MD1, Jennifer Zeng, BA1, Enrique Elli, MD2, Dawn Francis, MD1, Kenneth DeVault, MD2, Maoyin Pang, MD, PhD3
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Jacksonville, Jacksonville, FL; 3Mayo Clinic Florida, Jacksonville, FL
Introduction: Anti-reflux surgeries, including hiatal hernia repair (HHR), or fundoplication (F), improve acid reflux and decrease the need for proton-pump inhibitors (PPIs). Following surgery, most patients can discontinue PPIs. It remains unclear which factors are associated with the restarting of PPIs after their initial discontinuation. We aimed to determine features associated with the discontinuation and subsequent restarting of PPIs in patients with a hiatal hernia (HH) who undergo anti-reflux surgery.
Methods: We performed a retrospective study across four academic centers between January 2015 and December 2021 in patients with HH and GERD who underwent anti-reflux surgery, either HHR, F, or HHR+F. Wilcoxon Rank Sum and Fisher Exact Tests, and Kaplan-Meier Estimates with Cox Proportional Hazards Regression Analysis were utilized to determine features associated with PPI discontinuation and subsequent need to re-initiation. Statistical significance was defined as p< 0.10 given the small sample size. Statistical analysis was performed utilizing BlueSky Statistics software v. 7.0.
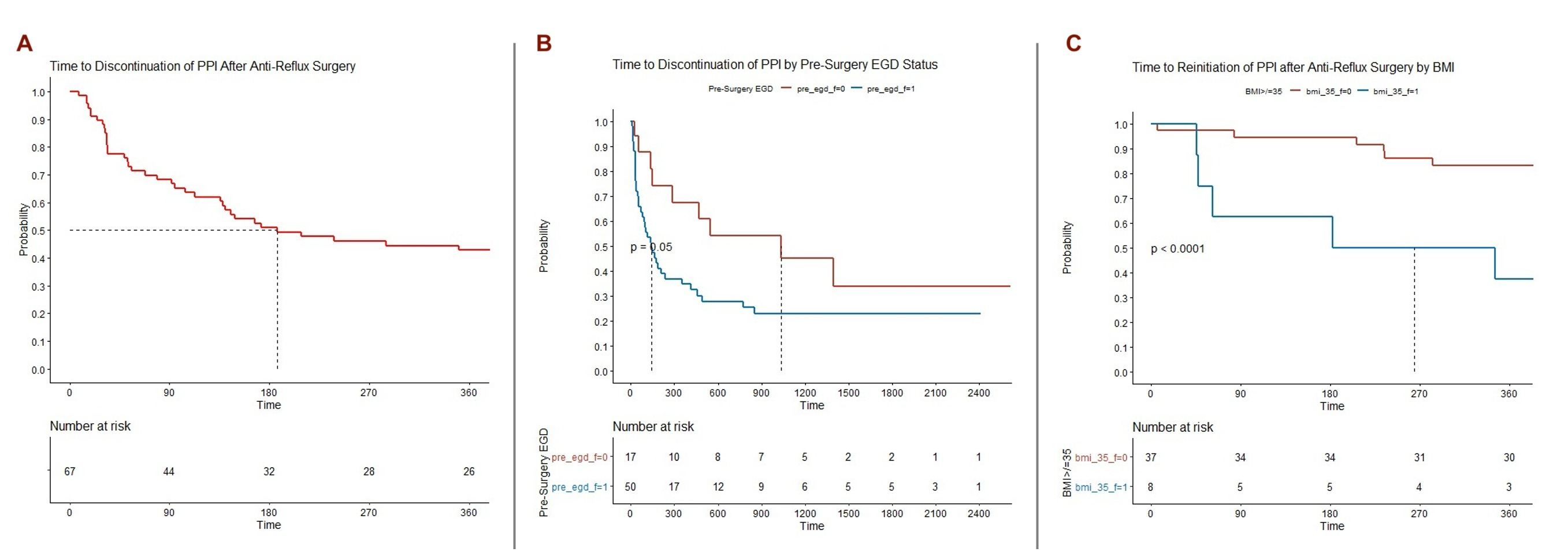
Results: A total of 75 patients were included. Table 1. Median times to PPI discontinuation and its subsequent restarting were 99.5 (IQR: 33.0-230.8) and 346.0 days (IQR: 183.0-880.0), respectively. At 3 months after surgery, being a never smoker, having had an upper endoscopy (EGD) or pH testing prior to surgery were associated with the initial discontinuation of PPI at p< 0.10. Having had an EGD increased the risk of discontinuation of PPI by 105%, p=0.0540. Body mass index (BMI), total percentage of acid exposure time, and DeMeester score were not associated with PPI discontinuation. After discontinuation, class II obesity or higher (BMI >/= 35.0 kg/m2) was very strongly associated with the restarting of PPI, p< 0.001. Every increase of 5 kg/m2 was associated with a 20% increased risk of needing to restart a PPI after anti-reflux surgery. Compared to HHR +/- F, a fundoplication alone increased the risk of restarting a PPI by 145% (HR 2.45, 95% CI: 0.92-6.49, p=0.0722). Figure 1. Having a large HH prior to surgery was not associated with restarting of PPI.
Discussion: We found increasing BMI, class II obesity of higher, and a fundoplication alone were the strongest predictors for needing to restart a PPI after anti-reflux surgery in patients with HH. Failure of the fundoplication due to increasing body mass causing increased intrathoracic pressure may explain this finding. Further research is recommended.
Disclosures:
Pedro Cortés, MD1, Jennifer Zeng, BA1, Enrique Elli, MD2, Dawn Francis, MD1, Kenneth DeVault, MD2, Maoyin Pang, MD, PhD3. C0205 - Fundoplication Alone and Class II Obesity or Higher Are Associated With the Need to Restart Proton Pump Inhibitors After Anti-Reflux Surgery in Patients With Hiatal Hernia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Jacksonville, Jacksonville, FL; 3Mayo Clinic Florida, Jacksonville, FL
Introduction: Anti-reflux surgeries, including hiatal hernia repair (HHR), or fundoplication (F), improve acid reflux and decrease the need for proton-pump inhibitors (PPIs). Following surgery, most patients can discontinue PPIs. It remains unclear which factors are associated with the restarting of PPIs after their initial discontinuation. We aimed to determine features associated with the discontinuation and subsequent restarting of PPIs in patients with a hiatal hernia (HH) who undergo anti-reflux surgery.
Methods: We performed a retrospective study across four academic centers between January 2015 and December 2021 in patients with HH and GERD who underwent anti-reflux surgery, either HHR, F, or HHR+F. Wilcoxon Rank Sum and Fisher Exact Tests, and Kaplan-Meier Estimates with Cox Proportional Hazards Regression Analysis were utilized to determine features associated with PPI discontinuation and subsequent need to re-initiation. Statistical significance was defined as p< 0.10 given the small sample size. Statistical analysis was performed utilizing BlueSky Statistics software v. 7.0.
Results: A total of 75 patients were included. Table 1. Median times to PPI discontinuation and its subsequent restarting were 99.5 (IQR: 33.0-230.8) and 346.0 days (IQR: 183.0-880.0), respectively. At 3 months after surgery, being a never smoker, having had an upper endoscopy (EGD) or pH testing prior to surgery were associated with the initial discontinuation of PPI at p< 0.10. Having had an EGD increased the risk of discontinuation of PPI by 105%, p=0.0540. Body mass index (BMI), total percentage of acid exposure time, and DeMeester score were not associated with PPI discontinuation. After discontinuation, class II obesity or higher (BMI >/= 35.0 kg/m2) was very strongly associated with the restarting of PPI, p< 0.001. Every increase of 5 kg/m2 was associated with a 20% increased risk of needing to restart a PPI after anti-reflux surgery. Compared to HHR +/- F, a fundoplication alone increased the risk of restarting a PPI by 145% (HR 2.45, 95% CI: 0.92-6.49, p=0.0722). Figure 1. Having a large HH prior to surgery was not associated with restarting of PPI.
Discussion: We found increasing BMI, class II obesity of higher, and a fundoplication alone were the strongest predictors for needing to restart a PPI after anti-reflux surgery in patients with HH. Failure of the fundoplication due to increasing body mass causing increased intrathoracic pressure may explain this finding. Further research is recommended.
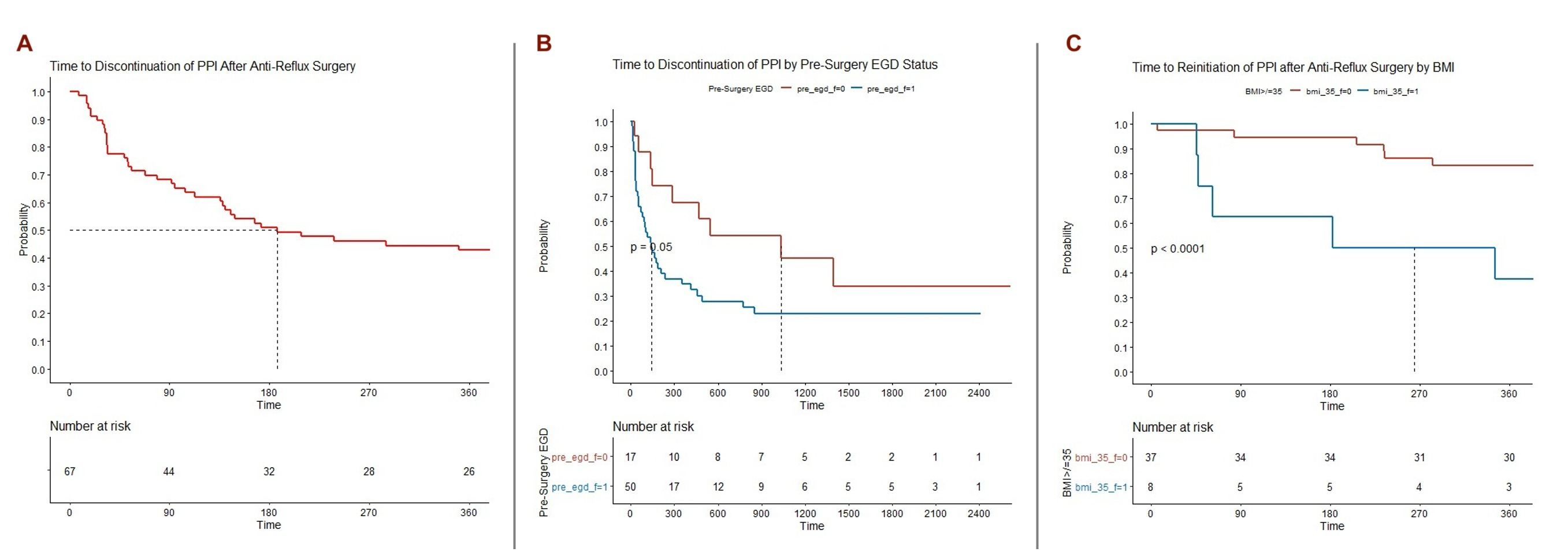
Figure: Figure 1: Kaplan-Meier Estimates of A) Time to Initial Discontinuation of PPI after Anti-Reflux Surgery in Patients with Hiatal Hernia, B) Time to Discontinuation of PPI by Pre-Surgery EGD, and C) Time to Restarting of PPI after Anti-Reflux Surgery by Class II Obesity or Higher (>/= 35.0 kg/m2). Legend A: Red = All Patients; Legend B: Blue = EGD Performed Prior to Surgery, Red = EGD Not Performed Prior to Surgery; Legend C: Blue = BMI >/= 35 kg/m2, Red = BMI < 35 kg/m2.
Table: Table 1: Baseline Characteristics According to Resolution of GERD at 1 Month after Anti-Reflux Surgery Followed by Cox Proportional Hazards Regression for Resolution of GERD and its Recurrence.
Disclosures:
Pedro Cortés indicated no relevant financial relationships.
Jennifer Zeng indicated no relevant financial relationships.
Enrique Elli indicated no relevant financial relationships.
Dawn Francis indicated no relevant financial relationships.
Kenneth DeVault indicated no relevant financial relationships.
Maoyin Pang indicated no relevant financial relationships.
Pedro Cortés, MD1, Jennifer Zeng, BA1, Enrique Elli, MD2, Dawn Francis, MD1, Kenneth DeVault, MD2, Maoyin Pang, MD, PhD3. C0205 - Fundoplication Alone and Class II Obesity or Higher Are Associated With the Need to Restart Proton Pump Inhibitors After Anti-Reflux Surgery in Patients With Hiatal Hernia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
