Back


Poster Session C - Monday Afternoon
Category: GI Bleeding
C0323 - Analysis of Trends in Mortality Rate, Racial Disparity, and Outcomes Among U.S. Patients Hospitalized for Bleeding Esophageal Varices: A Decade-Long Retrospective Study From the National Inpatient Sample Database
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio
- EE
Ebehiwele Ebhohon, MD, MPH
Lincoln Medical and Mental Health Center
Bronx, NY
Presenting Author(s)
Ebehiwele Ebhohon, MD, MPH1, Yassine Kilani, MD2, Olachi J. Egbo, MD3, Abdultawab Shaka, MBBS4, Pius Ojemolon, MBBS5, Robert Kwei-Nsoro, MD6, Hisham Laswi, MD7, Hafeez Shaka, MBBS7
1Lincoln Medical and Mental Health Center, Bronx, NY; 2NYCHHC/Lincoln Medical Center, Bronx, NY; 3Aurora Medical Center Oshkosh, Oshkosh, WI; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 5John H. Stroger Jr. Hospital of Cook County, Chicago, IL; 6John H. Stroger, Jr Hospital of Cook County, Chicago, IL; 7John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Bleeding esophageal varices (BEV) is a life-threatening condition historically associated with high mortality. Recent epidemiologic data stratified by sex and race on hospital outcomes over the past decade are lacking. Our study aimed to evaluate 10-year trends in sociodemographic differences in patients hospitalized for BEV among adults in the U.S.
Methods: This retrospective longitudinal study involved BEV hospitalizations in the U.S. using the National Inpatient Sample collected from 2010 to 2019. The outcomes evaluated in this study were sociodemographic differences in inpatient mortality rate, mean length of hospital stay (LOS), and mean total hospital charges (THC). We used Stata® Version 17 software (StataCorp, Texas, USA) and Joinpoint Regression Program, Version 4.9.1.0, for data analysis. We set a p-value of < 0.05 for statistical significance throughout the study.
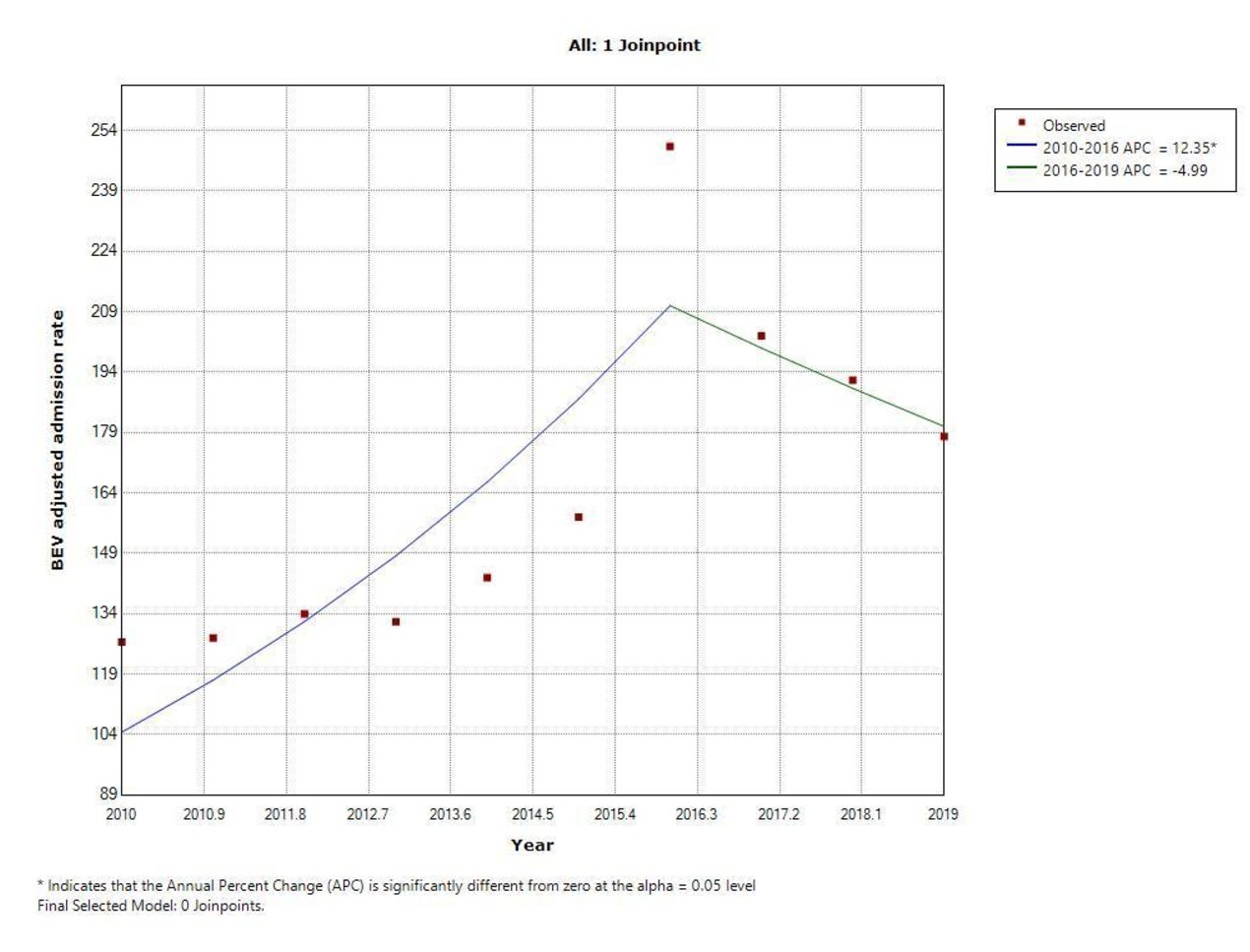
Results: From 2010 to 2019, there were 50,017 hospitalizations with a primary diagnosis of BEV. The BEV hospitalization appears to be highest among middle-aged whites, those with Medicare insurance, and hospitalization at large urban non-teaching centers. From 2010 to 2019, the BEV admission rate increased from 127 to 178 per million adult hospitalizations. Joinpoint analysis showed an average annual percent change of 6.2% (95% CI 4.4 – 8.2, p< 0.001). Over the period, mortality was 5.7% in males compared to 4.4% in females, 4.7% in Whites, 7.9% in Blacks, 5.0% in Hispanics, 5.8% in the low-income quartile, and 5.3% in the high-income quartile. Among the groups, only Hispanics significantly decreased mortality over the study period.
Discussion: The findings of this retrospective study suggest that the 10-year trend in mortality rate and LOS for BEV hospitalizations remain primarily unchanged. However, there was a significant increase in total hospital charges. Blacks, Males, and low-income quartile patients were likelier to have higher mortality rates from BEV than their comparison groups.
Disclosures:
Ebehiwele Ebhohon, MD, MPH1, Yassine Kilani, MD2, Olachi J. Egbo, MD3, Abdultawab Shaka, MBBS4, Pius Ojemolon, MBBS5, Robert Kwei-Nsoro, MD6, Hisham Laswi, MD7, Hafeez Shaka, MBBS7. C0323 - Analysis of Trends in Mortality Rate, Racial Disparity, and Outcomes Among U.S. Patients Hospitalized for Bleeding Esophageal Varices: A Decade-Long Retrospective Study From the National Inpatient Sample Database, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Lincoln Medical and Mental Health Center, Bronx, NY; 2NYCHHC/Lincoln Medical Center, Bronx, NY; 3Aurora Medical Center Oshkosh, Oshkosh, WI; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 5John H. Stroger Jr. Hospital of Cook County, Chicago, IL; 6John H. Stroger, Jr Hospital of Cook County, Chicago, IL; 7John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Bleeding esophageal varices (BEV) is a life-threatening condition historically associated with high mortality. Recent epidemiologic data stratified by sex and race on hospital outcomes over the past decade are lacking. Our study aimed to evaluate 10-year trends in sociodemographic differences in patients hospitalized for BEV among adults in the U.S.
Methods: This retrospective longitudinal study involved BEV hospitalizations in the U.S. using the National Inpatient Sample collected from 2010 to 2019. The outcomes evaluated in this study were sociodemographic differences in inpatient mortality rate, mean length of hospital stay (LOS), and mean total hospital charges (THC). We used Stata® Version 17 software (StataCorp, Texas, USA) and Joinpoint Regression Program, Version 4.9.1.0, for data analysis. We set a p-value of < 0.05 for statistical significance throughout the study.
Results: From 2010 to 2019, there were 50,017 hospitalizations with a primary diagnosis of BEV. The BEV hospitalization appears to be highest among middle-aged whites, those with Medicare insurance, and hospitalization at large urban non-teaching centers. From 2010 to 2019, the BEV admission rate increased from 127 to 178 per million adult hospitalizations. Joinpoint analysis showed an average annual percent change of 6.2% (95% CI 4.4 – 8.2, p< 0.001). Over the period, mortality was 5.7% in males compared to 4.4% in females, 4.7% in Whites, 7.9% in Blacks, 5.0% in Hispanics, 5.8% in the low-income quartile, and 5.3% in the high-income quartile. Among the groups, only Hispanics significantly decreased mortality over the study period.
Discussion: The findings of this retrospective study suggest that the 10-year trend in mortality rate and LOS for BEV hospitalizations remain primarily unchanged. However, there was a significant increase in total hospital charges. Blacks, Males, and low-income quartile patients were likelier to have higher mortality rates from BEV than their comparison groups.
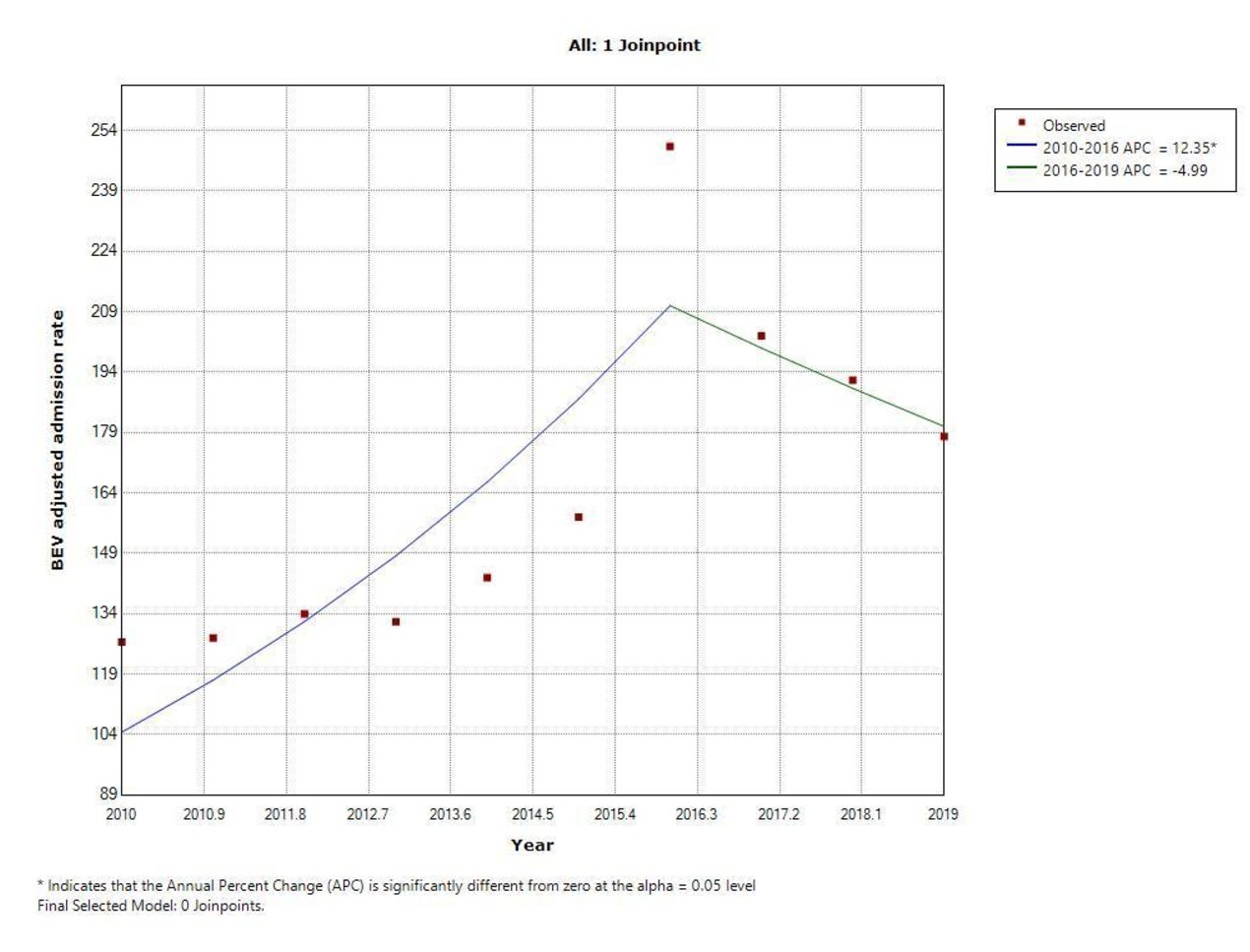
Figure: Figure 1: Trends in Adjusted BEV Hospitalization Rate from 2010 to 2019
Disclosures:
Ebehiwele Ebhohon indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Olachi Egbo indicated no relevant financial relationships.
Abdultawab Shaka indicated no relevant financial relationships.
Pius Ojemolon indicated no relevant financial relationships.
Robert Kwei-Nsoro indicated no relevant financial relationships.
Hisham Laswi indicated no relevant financial relationships.
Hafeez Shaka indicated no relevant financial relationships.
Ebehiwele Ebhohon, MD, MPH1, Yassine Kilani, MD2, Olachi J. Egbo, MD3, Abdultawab Shaka, MBBS4, Pius Ojemolon, MBBS5, Robert Kwei-Nsoro, MD6, Hisham Laswi, MD7, Hafeez Shaka, MBBS7. C0323 - Analysis of Trends in Mortality Rate, Racial Disparity, and Outcomes Among U.S. Patients Hospitalized for Bleeding Esophageal Varices: A Decade-Long Retrospective Study From the National Inpatient Sample Database, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
