Back

Poster Session C - Monday Afternoon
Category: GI Bleeding
C0331 - Meckel’s-Associated Polypoid Vascular Mass of the Small Bowel: A Case Report of Obscure-Overt GI Bleeding
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Rachel Hannum, MD
UPMC
Pittsburgh, PA
Presenting Author(s)
Rachel Hannum, MD, Charles Gabbert, MD
UPMC, Pittsburgh, PA
Introduction: Obscure-overt GI bleeding has traditionally been defined as recurrent visible bleeding that is not identified on standard endoscopy and colonoscopy, even radiographically. Small bowel angioectasias and NSAID ulcers are common in older adults, whereas younger patients frequently present with inflammatory bowel disease and polyp syndromes. We present a unique case of truly “obscure-overt” GI bleeding that was finally identified with retrograde double balloon enteroscopy (DBE).
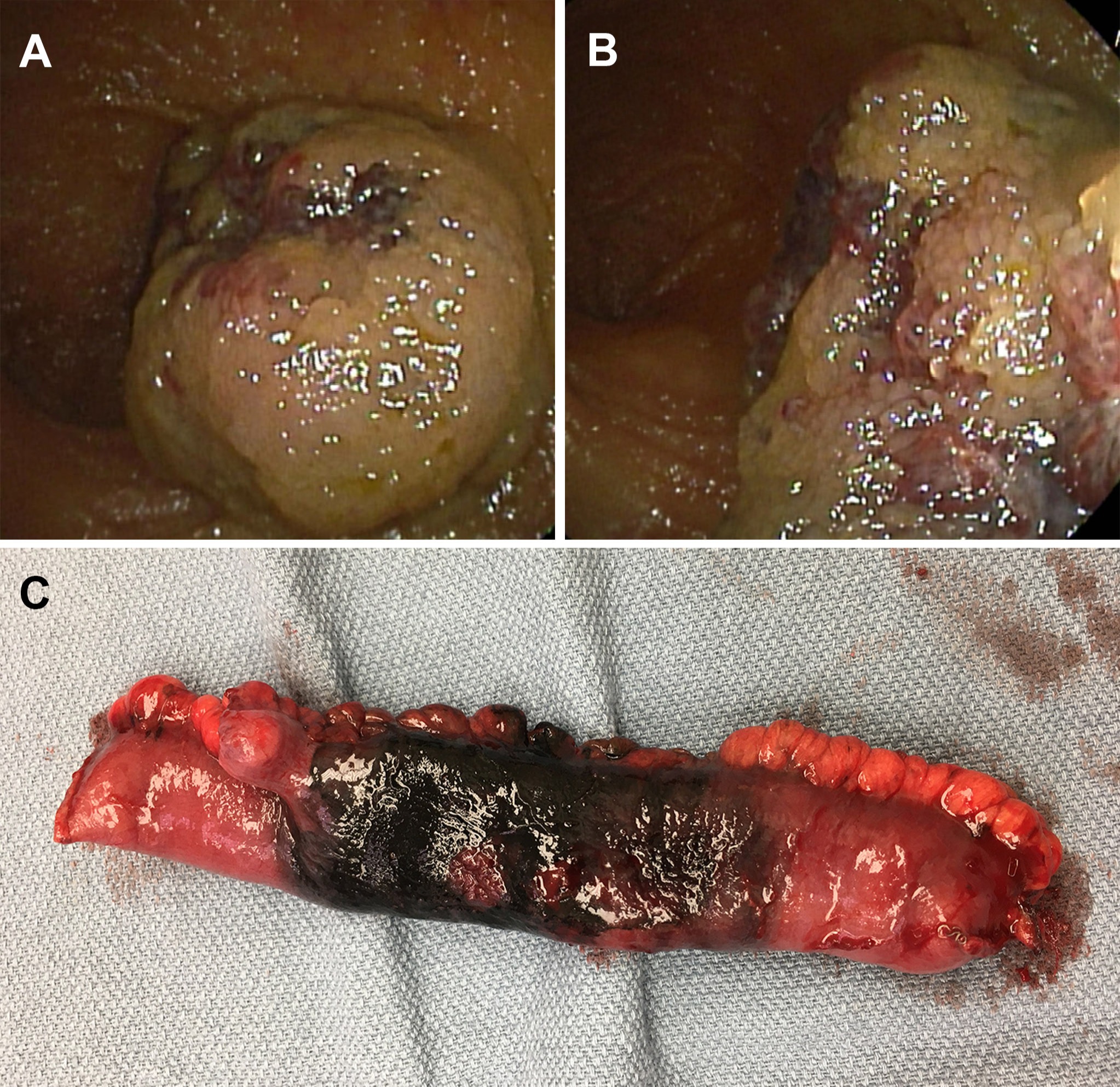
Case Description/Methods: 24-year-old male presents with intermittent maroon blood per rectum. His medical history includes two vascular malformations requiring surgical resection at an early age (large lesion on neck, small distal digit lesion). He reports prior episodes of GI bleeding requiring admission for endotherapy since the age of 15. Extensive evaluation at outside facilities included: multiple EGDs and colonoscopies, video capsule endoscopy (VCE), deep small bowel enteroscopy (anterograde and retrograde), a negative Meckel’s scan, and CT–angiograms without acute findings. On admission, he was found to have Hgb 5.6 and ferritin 2.0. VCE was repeated and revealed hematin with adjacent mucosal surface ulceration approximately one hour upstream of the ileocecal valve. Subsequent retrograde DBE identified a polypoid, vascular mass with stigmata of bleeding in the mid ileum (Figure 1a, b). The lesion was tattooed and hemoclips were placed to guide resection. Laparotomy for 13.5 cm small bowel resection revealed a nodular 2cm vascular malformation involving submucosal tissue and muscularis propria, with an associated Meckel’s diverticulum at the base of the mass (Figure 1c). The patient recovered from surgery uneventfully.
Discussion: Meckel’s diverticulum (MD) has been associated with malignancy, bleeding, and intussusception, as we present the only reported case of an associated polypoid vascular malformation resulting in recurrent bleeding. This case is unique due to young age, predisposition to vascular malformations, and the extensive investigation prior. While Meckel’s scan (MS) remains the gold standard for diagnosis, previous studies have shown DBE is more sensitive than MS, CT-angiogram, and VCE at identifying bleeding MDs.1 This case illustrates that DBE should be considered when atypical small bowel pathology is suspected despite a negative prior workup.
1. Fukushima, M. et al. A case series of Meckel's diverticulum: usefulness of double-balloon enteroscopy for diagnosis. 2014. BMC gastroenterology, 14, 155.
Disclosures:
Rachel Hannum, MD, Charles Gabbert, MD. C0331 - Meckel’s-Associated Polypoid Vascular Mass of the Small Bowel: A Case Report of Obscure-Overt GI Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
UPMC, Pittsburgh, PA
Introduction: Obscure-overt GI bleeding has traditionally been defined as recurrent visible bleeding that is not identified on standard endoscopy and colonoscopy, even radiographically. Small bowel angioectasias and NSAID ulcers are common in older adults, whereas younger patients frequently present with inflammatory bowel disease and polyp syndromes. We present a unique case of truly “obscure-overt” GI bleeding that was finally identified with retrograde double balloon enteroscopy (DBE).
Case Description/Methods: 24-year-old male presents with intermittent maroon blood per rectum. His medical history includes two vascular malformations requiring surgical resection at an early age (large lesion on neck, small distal digit lesion). He reports prior episodes of GI bleeding requiring admission for endotherapy since the age of 15. Extensive evaluation at outside facilities included: multiple EGDs and colonoscopies, video capsule endoscopy (VCE), deep small bowel enteroscopy (anterograde and retrograde), a negative Meckel’s scan, and CT–angiograms without acute findings. On admission, he was found to have Hgb 5.6 and ferritin 2.0. VCE was repeated and revealed hematin with adjacent mucosal surface ulceration approximately one hour upstream of the ileocecal valve. Subsequent retrograde DBE identified a polypoid, vascular mass with stigmata of bleeding in the mid ileum (Figure 1a, b). The lesion was tattooed and hemoclips were placed to guide resection. Laparotomy for 13.5 cm small bowel resection revealed a nodular 2cm vascular malformation involving submucosal tissue and muscularis propria, with an associated Meckel’s diverticulum at the base of the mass (Figure 1c). The patient recovered from surgery uneventfully.
Discussion: Meckel’s diverticulum (MD) has been associated with malignancy, bleeding, and intussusception, as we present the only reported case of an associated polypoid vascular malformation resulting in recurrent bleeding. This case is unique due to young age, predisposition to vascular malformations, and the extensive investigation prior. While Meckel’s scan (MS) remains the gold standard for diagnosis, previous studies have shown DBE is more sensitive than MS, CT-angiogram, and VCE at identifying bleeding MDs.1 This case illustrates that DBE should be considered when atypical small bowel pathology is suspected despite a negative prior workup.
1. Fukushima, M. et al. A case series of Meckel's diverticulum: usefulness of double-balloon enteroscopy for diagnosis. 2014. BMC gastroenterology, 14, 155.
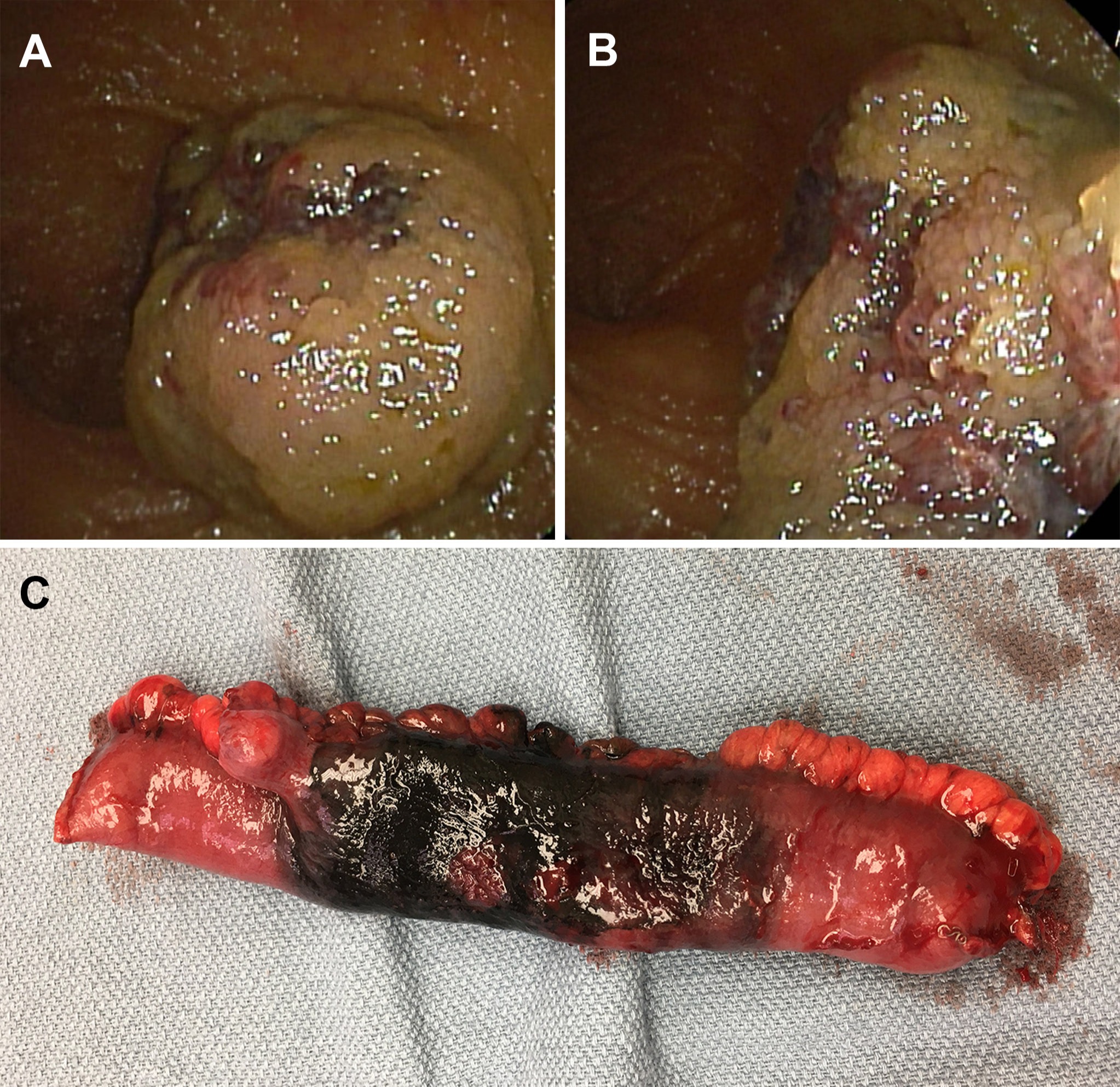
Figure: Figure 1. A: Retrograde double balloon enteroscopy image of the polypoid, nodular, vascular mass in the mid-ileum. B: Enteroscopy image of the vascular mass with stigmata of bleeding. C: Gross pathologic specimen of the 13.5cm small bowel resection with associated Meckel’s diverticulum directly adjacent to the tattooed tissue (left).
Disclosures:
Rachel Hannum indicated no relevant financial relationships.
Charles Gabbert indicated no relevant financial relationships.
Rachel Hannum, MD, Charles Gabbert, MD. C0331 - Meckel’s-Associated Polypoid Vascular Mass of the Small Bowel: A Case Report of Obscure-Overt GI Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
