Back

Poster Session C - Monday Afternoon
Category: Biliary/Pancreas
C0084 - Hypertriglyceridemia Independent Propofol-Induced Acute Pancreatitis – A Rare and Unusual Complication
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Peter Bhandari, MD
Northwell Health, Lenox Hill Hospital
New York, NY
Presenting Author(s)
Award: Presidential Poster Award
Peter Bhandari, MD1, Nicholas Condiles, MD2, Samip Shah, MD3, David H. Robbins, MD1
1Northwell Health, Lenox Hill Hospital, New York, NY; 2Northwell Health, New York, NY; 3Lenox Hill Hospital, New York, NY
Introduction: Propofol is a widely utilized lipophilic sedative anesthetic. Common side effects include hypotension, apnea, and rash. While rare, acute pancreatitis (AP) is a documented complication of propofol administration. Though the exact mechanism has yet to be established, current theories include propofol-induced hypertriglyceridemia (HTG) or idiosyncratic hypersensitivity reaction. We present a rare case of HTG-independent propofol-induced AP after an elective rhytidectomy.
Case Description/Methods: A 75-year-old woman with hypertension and hypothyroidism, presented with four days of worsening mentation, abdominal distention and pain after an outpatient rhytidectomy. She was a former smoker, but denied alcohol or illicit drug use. On arrival, vital signs were significant for fever of 100.4F and tachycardia to 106 beats/min. Physical exam was significant for abdominal distension and epigastric tenderness. Laboratory studies revealed leukocytosis of 12,200 mm3 with 10.4% bandemia, alkaline phosphatase of 143 U/L, serum calcium of 8.9 mg/dL, lipase of 222 U/L, and triglycerides of 111 mg/dL. Abdominal ultrasound was unremarkable without evidence of gallstones or biliary dilatation. A computed tomography of the abdomen revealed extensive peripancreatic fat stranding and fluid with homogenous parenchymal enhancement consistent with severe interstitial edematous AP. An infectious workup was unremarkable for a concomitant source. Medication reconciliation revealed no confounding medications known to cause pancreatitis.
She received intravenous fluids, proton pump inhibitor and pain regimen. Her diet was gradually advanced and she clinically improved over the next 48 hours with mentation returning to baseline. She was subsequently discharged home.
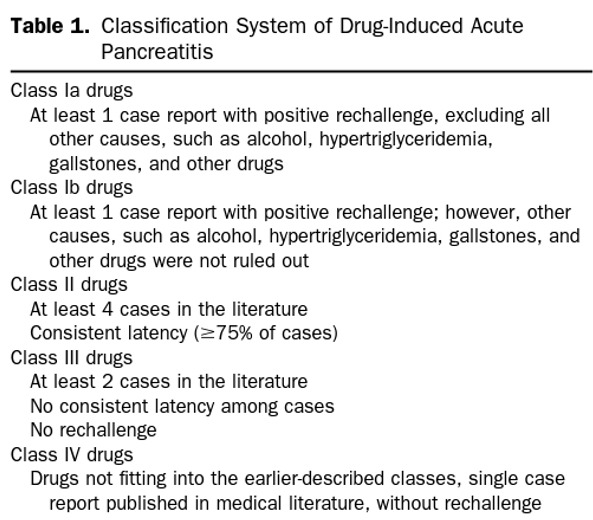
Discussion: AP is responsible for over 230,000 hospitalizations annually in the US, with drug-induced AP comprising 0.5-2% of all cases. Propofol-induced AP has been sparsely reported in the setting of HTG, though exceedingly rare without this lab abnormality. The Badalov classification system differentiates association and causality of drug-induced AP by evaluating latency, rechallenge, and published evidence (Table 1). Within this system, propofol has traditionally been characterized as a class II drug. However, recent published evidence has shown recurrence of AP upon propofol rechallenge, suggesting a more causal relation and a reclassification to class Ib. We present this case to raise awareness of the possible complications of propofol administration.
Disclosures:
Peter Bhandari, MD1, Nicholas Condiles, MD2, Samip Shah, MD3, David H. Robbins, MD1. C0084 - Hypertriglyceridemia Independent Propofol-Induced Acute Pancreatitis – A Rare and Unusual Complication, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Peter Bhandari, MD1, Nicholas Condiles, MD2, Samip Shah, MD3, David H. Robbins, MD1
1Northwell Health, Lenox Hill Hospital, New York, NY; 2Northwell Health, New York, NY; 3Lenox Hill Hospital, New York, NY
Introduction: Propofol is a widely utilized lipophilic sedative anesthetic. Common side effects include hypotension, apnea, and rash. While rare, acute pancreatitis (AP) is a documented complication of propofol administration. Though the exact mechanism has yet to be established, current theories include propofol-induced hypertriglyceridemia (HTG) or idiosyncratic hypersensitivity reaction. We present a rare case of HTG-independent propofol-induced AP after an elective rhytidectomy.
Case Description/Methods: A 75-year-old woman with hypertension and hypothyroidism, presented with four days of worsening mentation, abdominal distention and pain after an outpatient rhytidectomy. She was a former smoker, but denied alcohol or illicit drug use. On arrival, vital signs were significant for fever of 100.4F and tachycardia to 106 beats/min. Physical exam was significant for abdominal distension and epigastric tenderness. Laboratory studies revealed leukocytosis of 12,200 mm3 with 10.4% bandemia, alkaline phosphatase of 143 U/L, serum calcium of 8.9 mg/dL, lipase of 222 U/L, and triglycerides of 111 mg/dL. Abdominal ultrasound was unremarkable without evidence of gallstones or biliary dilatation. A computed tomography of the abdomen revealed extensive peripancreatic fat stranding and fluid with homogenous parenchymal enhancement consistent with severe interstitial edematous AP. An infectious workup was unremarkable for a concomitant source. Medication reconciliation revealed no confounding medications known to cause pancreatitis.
She received intravenous fluids, proton pump inhibitor and pain regimen. Her diet was gradually advanced and she clinically improved over the next 48 hours with mentation returning to baseline. She was subsequently discharged home.
Discussion: AP is responsible for over 230,000 hospitalizations annually in the US, with drug-induced AP comprising 0.5-2% of all cases. Propofol-induced AP has been sparsely reported in the setting of HTG, though exceedingly rare without this lab abnormality. The Badalov classification system differentiates association and causality of drug-induced AP by evaluating latency, rechallenge, and published evidence (Table 1). Within this system, propofol has traditionally been characterized as a class II drug. However, recent published evidence has shown recurrence of AP upon propofol rechallenge, suggesting a more causal relation and a reclassification to class Ib. We present this case to raise awareness of the possible complications of propofol administration.
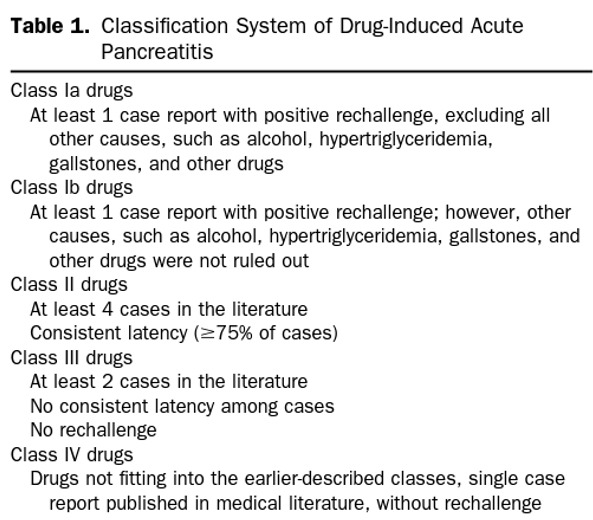
Figure: Table 1: The Badalov Classification System of Drug-Induced Acute Pancreatitis
Disclosures:
Peter Bhandari indicated no relevant financial relationships.
Nicholas Condiles indicated no relevant financial relationships.
Samip Shah indicated no relevant financial relationships.
David Robbins indicated no relevant financial relationships.
Peter Bhandari, MD1, Nicholas Condiles, MD2, Samip Shah, MD3, David H. Robbins, MD1. C0084 - Hypertriglyceridemia Independent Propofol-Induced Acute Pancreatitis – A Rare and Unusual Complication, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

