Back

Poster Session C - Monday Afternoon
Category: IBD
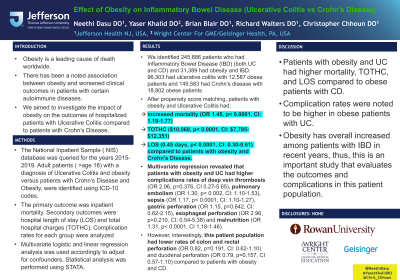
C0359 - Effect of Obesity on Inflammatory Bowel Disease (Ulcerative Colitis vs Crohn’s Disease)
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Neethi Dasu, DO
Jefferson Health New Jersey
Voorhees, NJ
Presenting Author(s)
Neethi Dasu, DO1, Yaser Khalid, DO2, Brian Blair, DO3, Richard Walters, DO4, Christopher Chhoun, DO5
1Jefferson Health New Jersey, Voorhees, NJ; 2Wright Center for GME/Geisinger Health System, Scranton, PA; 3Jefferson Health New Jersey, Cherry HIll, NJ; 4Jefferson Health New Jersey, Turnersville, NJ; 5Jefferson Health NJ, Voorhees, NJ
Introduction: Obesity is a leading cause of death worldwide. There has been a noted association between obesity and worsened clinical outcomes in patients with certain autoimmune diseases. We aimed to investigate the impact of obesity on the outcomes of hospitalized patients with Ulcerative Colitis compared to patients with Crohn’s Disease.
Methods: The National Inpatient Sample ( NIS) database was queried for the years 2015-2019. Adult patients ( >age 18) with a diagnosis of Ulcerative Colitis and obesity versus patients with Crohn’s Disease and Obesity, were identified using ICD-10 codes. The primary outcome was inpatient mortality. Secondary outcomes were hospital length of stay (LOS) and total hospital charges (TOTHC). Complication rates for each group were analyzed. Multivariate logistic and linear regression analysis was used accordingly to adjust for confounders. Statistical analysis was performed using STATA.
Results: We identified 245,886 patients who had Inflammatory Bowel Disease (IBD) (both UC and CD) and 31,389 had obesity and IBD. 96,303 had ulcerative colitis with 12,587 obese patients and 149,583 had Crohn’s disease with 18,802 obese patients. After propensity score matching, patients with obesity and Ulcerative Colitis had increased mortality (OR 1.45, p< 0.0001, CI: 1.19-1.77), TOTHC ($10,068, p< 0.0001, CI: $7,785-$12,351), and LOS (0.45 days, p< 0.0001, CI: 0.30-0.61) compared to patients with obesity and Crohn's Disease. Multivariate regression revealed that patients with obesity and UC had higher complications rates of deep vein thrombosis (OR 2.96, p=0.376, CI 0.27-5.65), pulmonary embolism (OR 1.30, p< 0.002, CI: 1.10-1.53), sepsis (OR 1.17, p< 0.0001, CI: 1.10-1.27), gastric perforation (OR 1.15, p=0.642, CI: 0.62-2.15), esophageal perforation (OR 2.96, p=0.210, CI: 0.54-5.38) and malnutrition (OR 1.31, p< 0.0001, CI 1.18-1.46). However, interestingly, this patient population had lower rates of colon and rectal perforation (OR 0.82, p=0.191, CI: 0.62-1.10) and duodenal perforation (OR 0.79, p=0.157, CI 0.57-1.10) compared to patients with obesity and CD.
Discussion: Patients with obesity and UC had higher mortality, TOTHC, and LOS compared to obese patients with CD. Complication rates were noted to be higher in obese patients with UC. Obesity has overall increased among patients with IBD in recent years, thus, this is an important study that evaluates the outcomes and complications in this patient population.
Disclosures:
Neethi Dasu, DO1, Yaser Khalid, DO2, Brian Blair, DO3, Richard Walters, DO4, Christopher Chhoun, DO5. C0359 - Effect of Obesity on Inflammatory Bowel Disease (Ulcerative Colitis vs Crohn’s Disease), ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Jefferson Health New Jersey, Voorhees, NJ; 2Wright Center for GME/Geisinger Health System, Scranton, PA; 3Jefferson Health New Jersey, Cherry HIll, NJ; 4Jefferson Health New Jersey, Turnersville, NJ; 5Jefferson Health NJ, Voorhees, NJ
Introduction: Obesity is a leading cause of death worldwide. There has been a noted association between obesity and worsened clinical outcomes in patients with certain autoimmune diseases. We aimed to investigate the impact of obesity on the outcomes of hospitalized patients with Ulcerative Colitis compared to patients with Crohn’s Disease.
Methods: The National Inpatient Sample ( NIS) database was queried for the years 2015-2019. Adult patients ( >age 18) with a diagnosis of Ulcerative Colitis and obesity versus patients with Crohn’s Disease and Obesity, were identified using ICD-10 codes. The primary outcome was inpatient mortality. Secondary outcomes were hospital length of stay (LOS) and total hospital charges (TOTHC). Complication rates for each group were analyzed. Multivariate logistic and linear regression analysis was used accordingly to adjust for confounders. Statistical analysis was performed using STATA.
Results: We identified 245,886 patients who had Inflammatory Bowel Disease (IBD) (both UC and CD) and 31,389 had obesity and IBD. 96,303 had ulcerative colitis with 12,587 obese patients and 149,583 had Crohn’s disease with 18,802 obese patients. After propensity score matching, patients with obesity and Ulcerative Colitis had increased mortality (OR 1.45, p< 0.0001, CI: 1.19-1.77), TOTHC ($10,068, p< 0.0001, CI: $7,785-$12,351), and LOS (0.45 days, p< 0.0001, CI: 0.30-0.61) compared to patients with obesity and Crohn's Disease. Multivariate regression revealed that patients with obesity and UC had higher complications rates of deep vein thrombosis (OR 2.96, p=0.376, CI 0.27-5.65), pulmonary embolism (OR 1.30, p< 0.002, CI: 1.10-1.53), sepsis (OR 1.17, p< 0.0001, CI: 1.10-1.27), gastric perforation (OR 1.15, p=0.642, CI: 0.62-2.15), esophageal perforation (OR 2.96, p=0.210, CI: 0.54-5.38) and malnutrition (OR 1.31, p< 0.0001, CI 1.18-1.46). However, interestingly, this patient population had lower rates of colon and rectal perforation (OR 0.82, p=0.191, CI: 0.62-1.10) and duodenal perforation (OR 0.79, p=0.157, CI 0.57-1.10) compared to patients with obesity and CD.
Discussion: Patients with obesity and UC had higher mortality, TOTHC, and LOS compared to obese patients with CD. Complication rates were noted to be higher in obese patients with UC. Obesity has overall increased among patients with IBD in recent years, thus, this is an important study that evaluates the outcomes and complications in this patient population.
Disclosures:
Neethi Dasu indicated no relevant financial relationships.
Yaser Khalid indicated no relevant financial relationships.
Brian Blair indicated no relevant financial relationships.
Richard Walters indicated no relevant financial relationships.
Christopher Chhoun indicated no relevant financial relationships.
Neethi Dasu, DO1, Yaser Khalid, DO2, Brian Blair, DO3, Richard Walters, DO4, Christopher Chhoun, DO5. C0359 - Effect of Obesity on Inflammatory Bowel Disease (Ulcerative Colitis vs Crohn’s Disease), ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
