Back

Poster Session A - Sunday Afternoon
Category: Liver
A0561 - A Rare Case of Vanishing Bile Duct Syndrome in a Patient With Sarcoidosis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Annie Shergill, MD
Larkin Community Hospital
Fresno, CA
Presenting Author(s)
Annie Shergill, MD
Larkin Community Hospital, Fresno, CA
Introduction: Vanishing Bile Duct Syndrome (VBDS) is an uncommon, acquired, chronic cholestatic liver disease mostly caused by drug induced liver injury, autoimmune disorders, malignancy and infectious causes. It presents with symptoms of cholestasis such as jaundice, pruritus and abnormal liver enzymes. Sarcoidosis is not known to commonly cause VBDS. We present a unique case of VBDS as a hepatic manifestation of sarcoidosis.
Case Description/Methods: A 39-year-old male with no significant past medical history presented with recurrent epistaxis, pruritus and was discovered to have a right nasal mass. Maxillofacial computed tomography (CT) revealed a nodular lesion in the nose with some bony erosions and multiple nodules in the parotid gland. Chest CT showed mediastinal lymphadenopathy. Biopsy of nasal mass showed focally necrotizing granulomatous inflammation without evidence of vasculitis consistent with sarcoidosis. Biopsy cultures were negative. He also had a history of getting recent tattoos which were found to be partially scarred and nodular. He did not report any significant alcohol use. Hepatitis B and C serologies were negative. Routine bloodwork revealed elevated liver enzymes: Total Bilirubin 1.0 mg/dl (direct 0.4), AST 270 units/L, ALT 316 units/L, Alk Phos 421 units/L, and GGT of 1425 units/L. Abdominal and pelvic CT showed hepatic morphology consistent with cirrhosis. Chronic liver disease workup included IgG level of 1680 mg/dL, but normal IgG4 level of 59.1 mg/dL, negative ANA, negative AMA and an ACE level of 65 mcg/L. Liver biopsy results showed significant ductopenia (approximately 75% of sampled portal tracts), mild portal, focal interface chronic inflammation and mild periportal fibrosis with delicate non-bridging septae, confirming a diagnosis of VBDS. The patient was treated with ursodexycholic acid and mycophenolate with significant improvement in his symptoms and liver enzymes.
Discussion: VBDS has rarely been associated with sarcoidosis. The most common hepatic manifestation in sarcoidosis is hepatic granulomas. However, in this case the liver biopsy did not show any sarcoid lesions but instead showed severe ductopenia consistent with VBDS. VBDS is characterized by bile duct paucity secondary to biliary apoptosis triggered by oxidative stress, drug induced injury and down regulation of B cell lymphoma-2 proteins. Hepatic involvement in sarcoidosis should be evaluated with a liver biopsy to elucidate causes such as VBDS as it changes the therapeutic management for the patient.
Disclosures:
Annie Shergill, MD. A0561 - A Rare Case of Vanishing Bile Duct Syndrome in a Patient With Sarcoidosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Larkin Community Hospital, Fresno, CA
Introduction: Vanishing Bile Duct Syndrome (VBDS) is an uncommon, acquired, chronic cholestatic liver disease mostly caused by drug induced liver injury, autoimmune disorders, malignancy and infectious causes. It presents with symptoms of cholestasis such as jaundice, pruritus and abnormal liver enzymes. Sarcoidosis is not known to commonly cause VBDS. We present a unique case of VBDS as a hepatic manifestation of sarcoidosis.
Case Description/Methods: A 39-year-old male with no significant past medical history presented with recurrent epistaxis, pruritus and was discovered to have a right nasal mass. Maxillofacial computed tomography (CT) revealed a nodular lesion in the nose with some bony erosions and multiple nodules in the parotid gland. Chest CT showed mediastinal lymphadenopathy. Biopsy of nasal mass showed focally necrotizing granulomatous inflammation without evidence of vasculitis consistent with sarcoidosis. Biopsy cultures were negative. He also had a history of getting recent tattoos which were found to be partially scarred and nodular. He did not report any significant alcohol use. Hepatitis B and C serologies were negative. Routine bloodwork revealed elevated liver enzymes: Total Bilirubin 1.0 mg/dl (direct 0.4), AST 270 units/L, ALT 316 units/L, Alk Phos 421 units/L, and GGT of 1425 units/L. Abdominal and pelvic CT showed hepatic morphology consistent with cirrhosis. Chronic liver disease workup included IgG level of 1680 mg/dL, but normal IgG4 level of 59.1 mg/dL, negative ANA, negative AMA and an ACE level of 65 mcg/L. Liver biopsy results showed significant ductopenia (approximately 75% of sampled portal tracts), mild portal, focal interface chronic inflammation and mild periportal fibrosis with delicate non-bridging septae, confirming a diagnosis of VBDS. The patient was treated with ursodexycholic acid and mycophenolate with significant improvement in his symptoms and liver enzymes.
Discussion: VBDS has rarely been associated with sarcoidosis. The most common hepatic manifestation in sarcoidosis is hepatic granulomas. However, in this case the liver biopsy did not show any sarcoid lesions but instead showed severe ductopenia consistent with VBDS. VBDS is characterized by bile duct paucity secondary to biliary apoptosis triggered by oxidative stress, drug induced injury and down regulation of B cell lymphoma-2 proteins. Hepatic involvement in sarcoidosis should be evaluated with a liver biopsy to elucidate causes such as VBDS as it changes the therapeutic management for the patient.
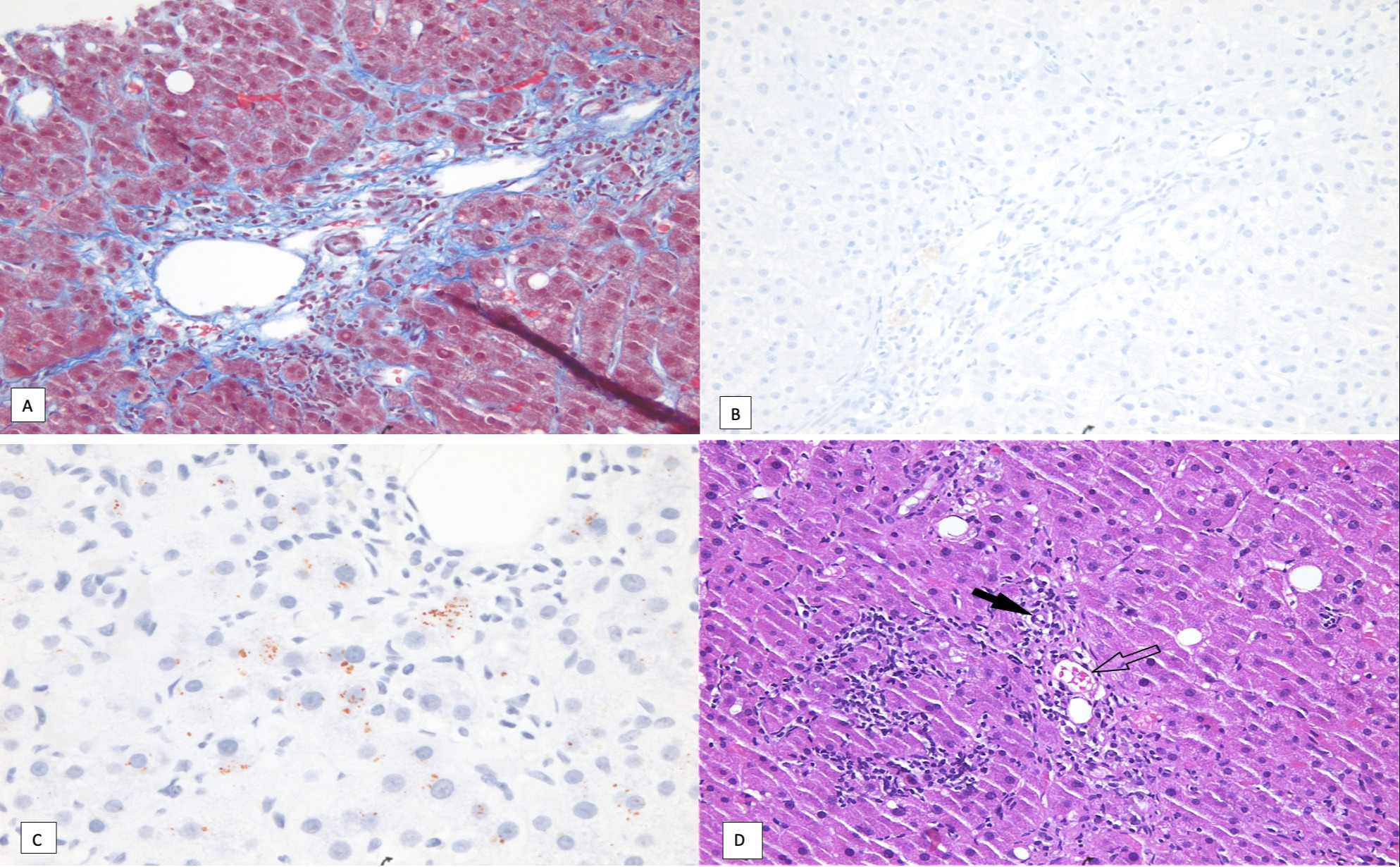
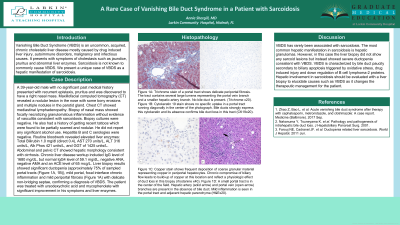
Figure: Figure 1A: Trichrome stain of a portal tract shows delicate periportal fibrosis. The tract contains several large lumens representing the portal vein branch and a smaller hepatic artery branch. No bile duct is present. (Trichrome x20).
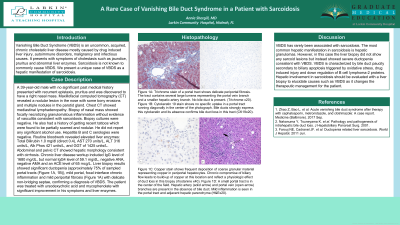
Figure 1B: Cytokeratin 19 stain shows no specific uptake in a portal tract running diagonally in the center of the photograph. Bile ducts strongly express this cytokeratin and its absence confirms bile duct loss in this tract (CK19x20).
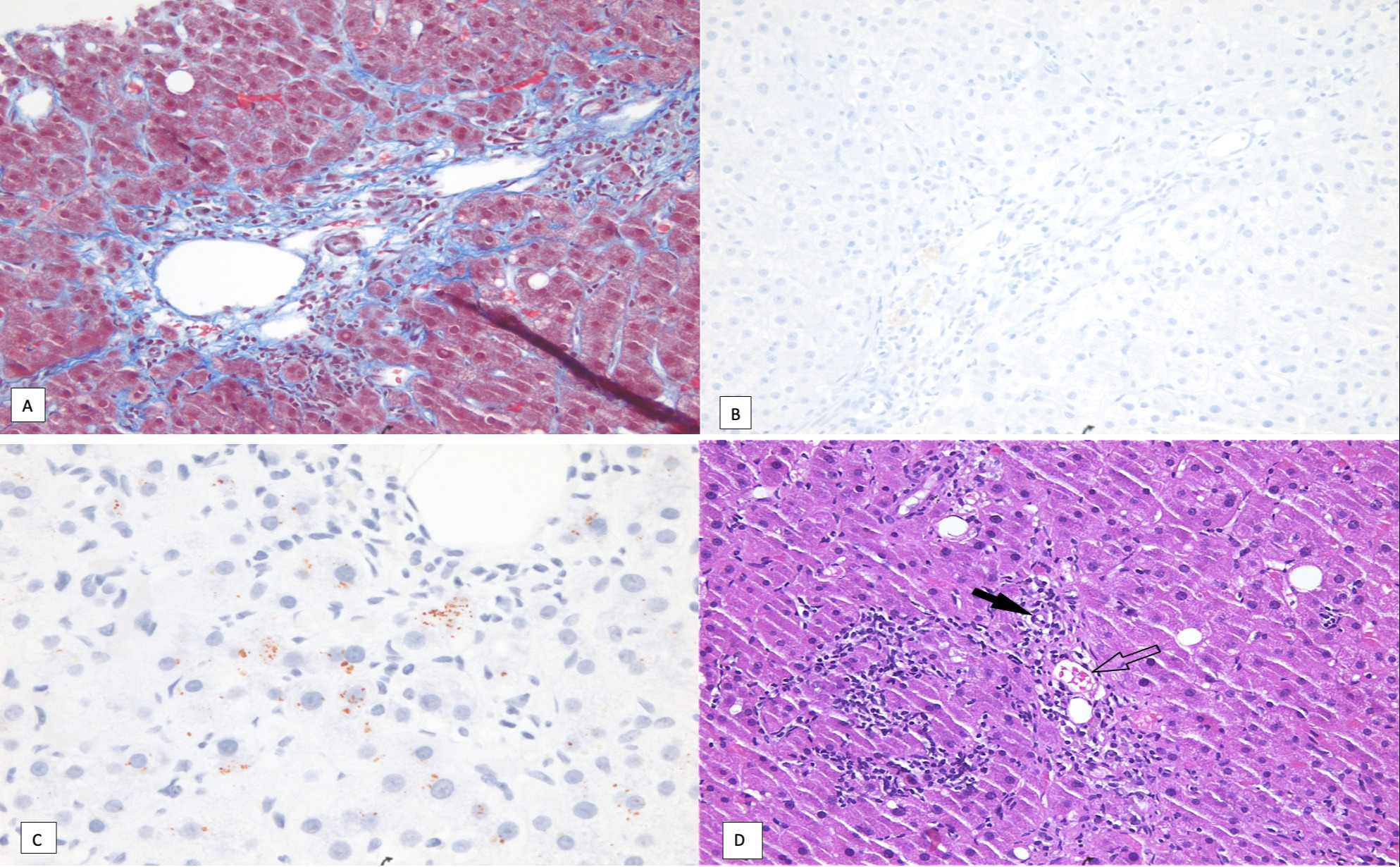
Figure 1C: Copper stain shows frequent deposition of coarse granular material representing copper in periportal hepatocytes. Chronic compromise of biliary flow leads to build-up of copper at this location and reflect a physiologic effect of duct loss in this biopsy (rhodanine x40).
Figure 1D: A small portal tract is in the center of the field. Hepatic artery (solid arrow) and portal vein (open arrow) branches are present in the absence of bile duct. Mild inflammation is seen in the portal tract and adjacent hepatic parenchyma (H&Ex20).
Figure 1B: Cytokeratin 19 stain shows no specific uptake in a portal tract running diagonally in the center of the photograph. Bile ducts strongly express this cytokeratin and its absence confirms bile duct loss in this tract (CK19x20).
Figure 1C: Copper stain shows frequent deposition of coarse granular material representing copper in periportal hepatocytes. Chronic compromise of biliary flow leads to build-up of copper at this location and reflect a physiologic effect of duct loss in this biopsy (rhodanine x40).
Figure 1D: A small portal tract is in the center of the field. Hepatic artery (solid arrow) and portal vein (open arrow) branches are present in the absence of bile duct. Mild inflammation is seen in the portal tract and adjacent hepatic parenchyma (H&Ex20).
Disclosures:
Annie Shergill indicated no relevant financial relationships.
Annie Shergill, MD. A0561 - A Rare Case of Vanishing Bile Duct Syndrome in a Patient With Sarcoidosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
