Back

Poster Session A - Sunday Afternoon
Category: Small Intestine
A0668 - Gastrointestinal Involvement With Vasculitis: A Rare and Difficult Distinction Between Intestinal Tuberculosis and Inflammatory Bowel Disease
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Daniel J. Ramirez, MS, DO
Genesys Regional Medical Center
Grand Blanc, MI
Presenting Author(s)
Daniel J. Ramirez, MS, DO1, Mark J. Minaudo, DO2
1Genesys Regional Medical Center, Grand Blanc, MI; 2Ascension Genesys Hospital, Grand Blanc, MI
Introduction: GI involvement is common in forms of vasculitis and presentation can mimic Inflammatory Bowel Disease (IBD) and infectious enteritis. We describe a 43 year old female with a history of Tuberculosis (TB) who presented with symptoms of IBD. Endoscopy showed circumferential ileal inflammation with biopsies ruling out Crohn’s Disease and microorganisms. Serology and kidney biopsy revealed P-ANCA positive Crescentic glomerulonephritis and Drug-Induced SLE and treatment included plasmapheresis, steroid taper and mycophenolate.
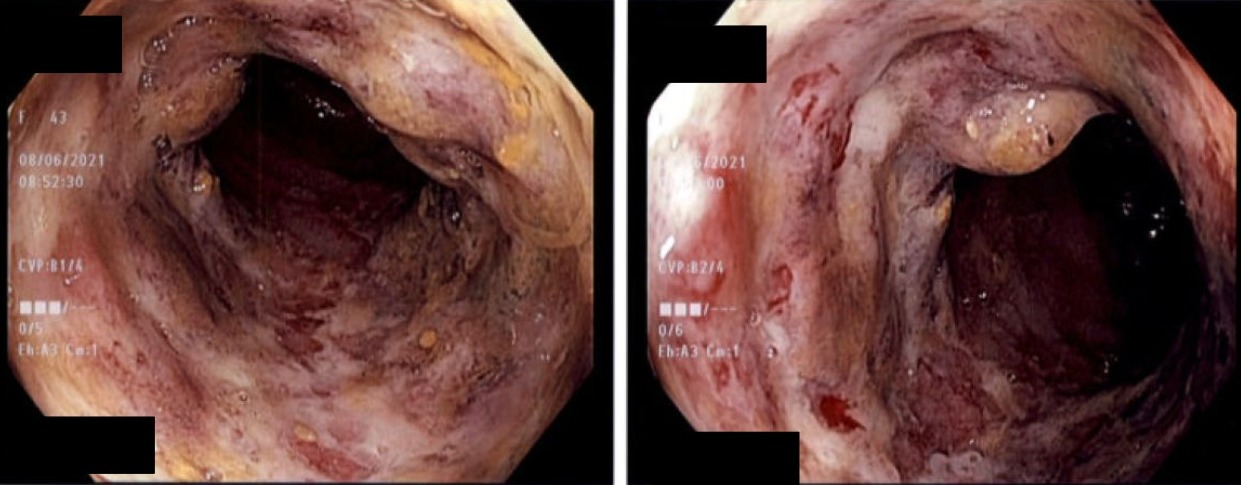
Case Description/Methods: A 43 year old female with a history of latent TB had recently discontinued Isoniazid due to adverse effects of abdominal pain and nausea. She presented with worsening abdominal pain and initial labs of anemia (hgb 6.9 g/dL), CRP 44.37 mg/L, ESR 80 mm/hr, Fecal Calprotectin 375 ug/mg and creatinine 2.49 mg/dL. CT showed retroperitoneal lymphadenopathy, multiple calcified lymph nodes, and thickened terminal ileum. Colonoscopy exposed 5-7 cm of continuous ileal ulcerative inflammation with spontaneous bleeding (Figure A) with biopsies positive for increased neutrophils and negative for Chron’s and microorganisms. Worsening kidney injury required dialysis. Serology was positive for P-ANCA and renal biopsy showed Crescentic Glomerulonephritis with segmental sclerosis, interstitial fibrosis and tubular atrophy. She was treated with plasmapheresis and steroids and was evaluated at a tertiary center where they diagnosed drug-induced SLE. Treatment included mycophenolate, prophylactic Bactrim and steroid taper.
Discussion: Blood vessel inflammation occurs in vasculitis with various forms inducing GI symptoms and kidney injury. Abdominal pain is the most common symptom followed by GI bleeding. This clinically overlaps with IBD and Intestinal Tuberculosis (ITB) as they all primarily affect the ileocecal region in young females. They differ histologically with ITB having large caseating granulomas and AFB stain, vasculitis with leukocytoclastic infiltrate, and Crohn's with non-caseating granulomas. There are no standardized treatments for GI vasculitis. Therapies reported include steroids, 5-ASA, Anti-TNF, cyclophosphamide, IVIG and plasmapheresis. Surgical management is conservative, with perforation being managed by resection. The diagnosis of GI vasculitis has historically been difficult and can be life threatening if missed. This carries high importance in endemic areas of TB and vasculitis and providing awareness may eliminate late diagnosis and surgery.
Disclosures:
Daniel J. Ramirez, MS, DO1, Mark J. Minaudo, DO2. A0668 - Gastrointestinal Involvement With Vasculitis: A Rare and Difficult Distinction Between Intestinal Tuberculosis and Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Genesys Regional Medical Center, Grand Blanc, MI; 2Ascension Genesys Hospital, Grand Blanc, MI
Introduction: GI involvement is common in forms of vasculitis and presentation can mimic Inflammatory Bowel Disease (IBD) and infectious enteritis. We describe a 43 year old female with a history of Tuberculosis (TB) who presented with symptoms of IBD. Endoscopy showed circumferential ileal inflammation with biopsies ruling out Crohn’s Disease and microorganisms. Serology and kidney biopsy revealed P-ANCA positive Crescentic glomerulonephritis and Drug-Induced SLE and treatment included plasmapheresis, steroid taper and mycophenolate.
Case Description/Methods: A 43 year old female with a history of latent TB had recently discontinued Isoniazid due to adverse effects of abdominal pain and nausea. She presented with worsening abdominal pain and initial labs of anemia (hgb 6.9 g/dL), CRP 44.37 mg/L, ESR 80 mm/hr, Fecal Calprotectin 375 ug/mg and creatinine 2.49 mg/dL. CT showed retroperitoneal lymphadenopathy, multiple calcified lymph nodes, and thickened terminal ileum. Colonoscopy exposed 5-7 cm of continuous ileal ulcerative inflammation with spontaneous bleeding (Figure A) with biopsies positive for increased neutrophils and negative for Chron’s and microorganisms. Worsening kidney injury required dialysis. Serology was positive for P-ANCA and renal biopsy showed Crescentic Glomerulonephritis with segmental sclerosis, interstitial fibrosis and tubular atrophy. She was treated with plasmapheresis and steroids and was evaluated at a tertiary center where they diagnosed drug-induced SLE. Treatment included mycophenolate, prophylactic Bactrim and steroid taper.
Discussion: Blood vessel inflammation occurs in vasculitis with various forms inducing GI symptoms and kidney injury. Abdominal pain is the most common symptom followed by GI bleeding. This clinically overlaps with IBD and Intestinal Tuberculosis (ITB) as they all primarily affect the ileocecal region in young females. They differ histologically with ITB having large caseating granulomas and AFB stain, vasculitis with leukocytoclastic infiltrate, and Crohn's with non-caseating granulomas. There are no standardized treatments for GI vasculitis. Therapies reported include steroids, 5-ASA, Anti-TNF, cyclophosphamide, IVIG and plasmapheresis. Surgical management is conservative, with perforation being managed by resection. The diagnosis of GI vasculitis has historically been difficult and can be life threatening if missed. This carries high importance in endemic areas of TB and vasculitis and providing awareness may eliminate late diagnosis and surgery.
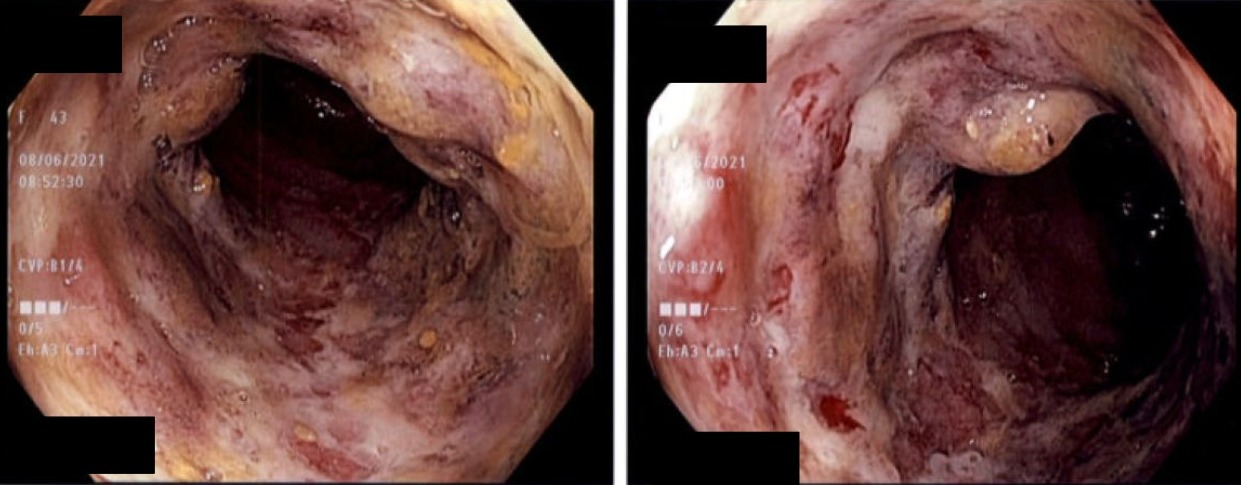
Figure: The small bowel was intubated showing a normal distal ileum however the following 5-7 cm of small bowel showed continuous severe ulcerative inflammation with erythema and spontaneous bleeding. More proximally, the ileal mucosa was again normal appearing.
Disclosures:
Daniel Ramirez indicated no relevant financial relationships.
Mark Minaudo indicated no relevant financial relationships.
Daniel J. Ramirez, MS, DO1, Mark J. Minaudo, DO2. A0668 - Gastrointestinal Involvement With Vasculitis: A Rare and Difficult Distinction Between Intestinal Tuberculosis and Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
