Back
Poster Session A - Sunday Afternoon
Category: Liver
A0575 - A Rare Case of Antiphospholipid Syndrome Presenting With Variceal Bleeding and Ascites Secondary to Portal Vein Thrombosis Without Liver Cirrhosis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Ahmed Eltelbany, MD, MPH
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Ahmed Eltelbany, MD, MPH, Rama Nanah, MD, Osama Hamid, MD, MRCPI, Sushrut Trakroo, MD, Khaled Alsabbagh Alchirazi, MD, M Housam Nanah, MD, Omar Massoud, MD
Cleveland Clinic, Cleveland, OH
Introduction: Portal vein thrombosis (PVT) mostly occurs with cirrhosis of the liver. However, it can also rarely occur without an associated liver disease. We present a case of PVT complicated by ascites and esophageal varices in the setting of antiphospholipid syndrome (APLS).
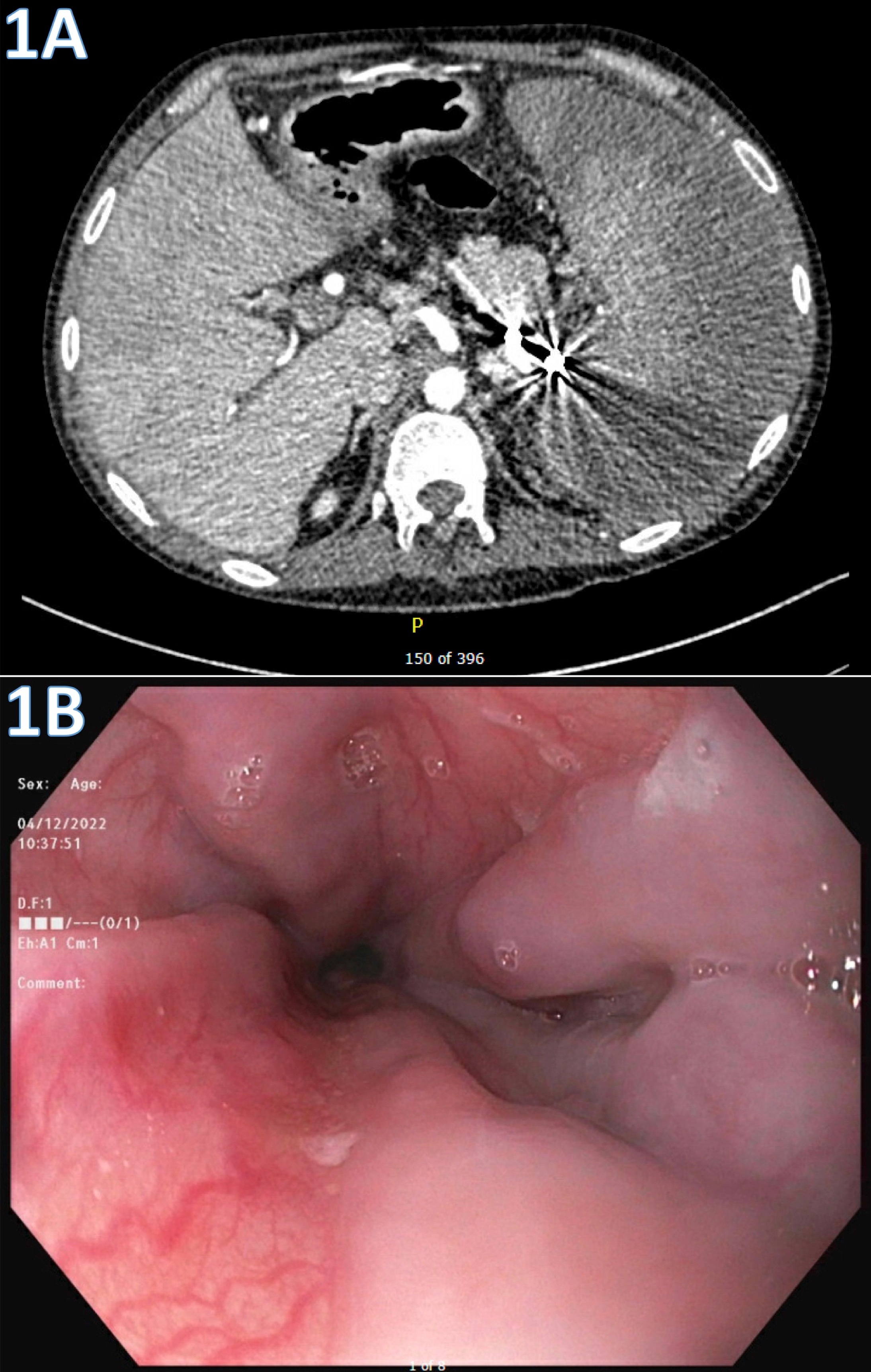
Case Description/Methods: A 31-year-old male with a history of ulcerative colitis and anti-phospholipid syndrome presented to the hospital after experiencing abdominal distension and upper gastrointestinal bleeding. Initial lab results revealed a hemoglobin of 6.4 g/dL. An abdominal CT showed heterogenous enhancement of liver parenchyma and extensive chronic portal venous system thrombosis with collaterals and splenomegaly with multiple infarcts (Figure 1A). Esophagogastroduodenoscopy (EGD) revealed non-bleeding grade I and small esophageal varices and type 1 gastroesophageal varies (Figure 1B). Patient was transfused packed red blood cells and underwent paracentesis with 4 liters drained. Liver ultrasound revealed mildly heterogenous liver with slightly increased echogenicity and chronically thrombosed left portal vein branch. Given the unclear etiology of PVT, a trans-jugular liver biopsy was completed and revealed mild steatosis and normal portal pressure of 8mmHg. Hospitalization was also complicated by splenic rupture and underwent embolization.
Discussion: PVT in the absence of cirrhosis is rare. In this case, the etiology of PVT is thought to be secondary to the hypercoagulable state in APLS. Ascites is a common symptom in patients with portal hypertension secondary to cirrhosis, however our patient was found to have ascites secondary to PVT in the absence of cirrhosis. Furthermore, PVT in APLS has been very rarely reported and may thus lead to PVT underdiagnosis or misdiagnosis at first. The most common presentation of PVT is variceal bleeding followed by pancytopenia due to hypersplenism while symptomatic portal hypertension is often indicative of the late stage of the PVT. Management is controversial and typically depends on the acuity of the thrombi. Anticoagulation therapy (AC) is generally warranted and may lead to significantly high rates of thrombus re-canalization. However, a significant cause of mortality in PVT is caused by variceal bleeding. It is important to recognize portal vein thrombosis as an alternative etiology of ascites in patients without evidence of cirrhosis and carefully time AC for improved outcomes.
Disclosures:
Ahmed Eltelbany, MD, MPH, Rama Nanah, MD, Osama Hamid, MD, MRCPI, Sushrut Trakroo, MD, Khaled Alsabbagh Alchirazi, MD, M Housam Nanah, MD, Omar Massoud, MD. A0575 - A Rare Case of Antiphospholipid Syndrome Presenting With Variceal Bleeding and Ascites Secondary to Portal Vein Thrombosis Without Liver Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Cleveland Clinic, Cleveland, OH
Introduction: Portal vein thrombosis (PVT) mostly occurs with cirrhosis of the liver. However, it can also rarely occur without an associated liver disease. We present a case of PVT complicated by ascites and esophageal varices in the setting of antiphospholipid syndrome (APLS).
Case Description/Methods: A 31-year-old male with a history of ulcerative colitis and anti-phospholipid syndrome presented to the hospital after experiencing abdominal distension and upper gastrointestinal bleeding. Initial lab results revealed a hemoglobin of 6.4 g/dL. An abdominal CT showed heterogenous enhancement of liver parenchyma and extensive chronic portal venous system thrombosis with collaterals and splenomegaly with multiple infarcts (Figure 1A). Esophagogastroduodenoscopy (EGD) revealed non-bleeding grade I and small esophageal varices and type 1 gastroesophageal varies (Figure 1B). Patient was transfused packed red blood cells and underwent paracentesis with 4 liters drained. Liver ultrasound revealed mildly heterogenous liver with slightly increased echogenicity and chronically thrombosed left portal vein branch. Given the unclear etiology of PVT, a trans-jugular liver biopsy was completed and revealed mild steatosis and normal portal pressure of 8mmHg. Hospitalization was also complicated by splenic rupture and underwent embolization.
Discussion: PVT in the absence of cirrhosis is rare. In this case, the etiology of PVT is thought to be secondary to the hypercoagulable state in APLS. Ascites is a common symptom in patients with portal hypertension secondary to cirrhosis, however our patient was found to have ascites secondary to PVT in the absence of cirrhosis. Furthermore, PVT in APLS has been very rarely reported and may thus lead to PVT underdiagnosis or misdiagnosis at first. The most common presentation of PVT is variceal bleeding followed by pancytopenia due to hypersplenism while symptomatic portal hypertension is often indicative of the late stage of the PVT. Management is controversial and typically depends on the acuity of the thrombi. Anticoagulation therapy (AC) is generally warranted and may lead to significantly high rates of thrombus re-canalization. However, a significant cause of mortality in PVT is caused by variceal bleeding. It is important to recognize portal vein thrombosis as an alternative etiology of ascites in patients without evidence of cirrhosis and carefully time AC for improved outcomes.
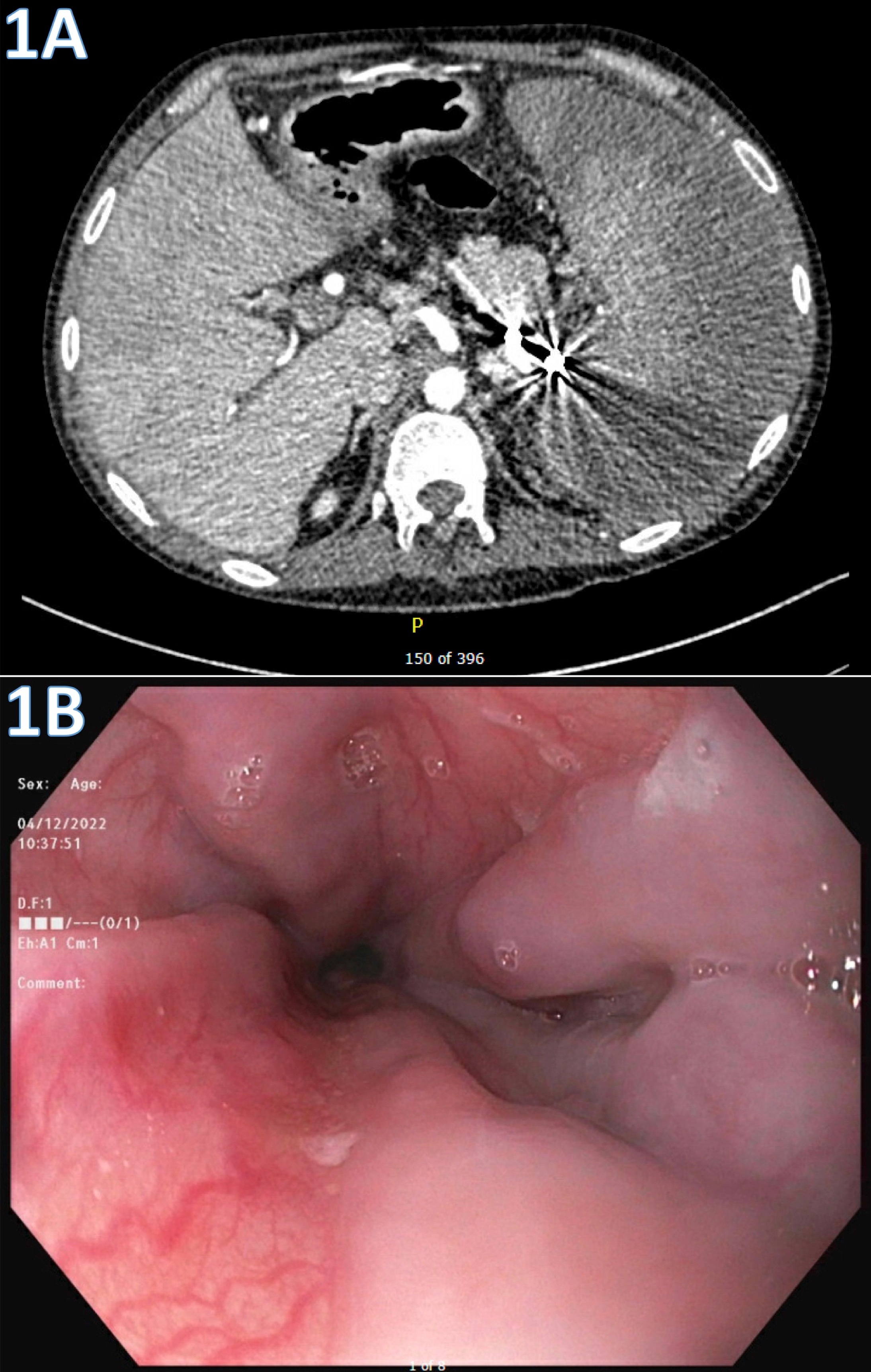
Figure: Figure 1: A) Transverse CT abdomen demonstrating large portal vein thrombosis B) Endoscopy image of the of the esophagus with varices
Disclosures:
Ahmed Eltelbany indicated no relevant financial relationships.
Rama Nanah indicated no relevant financial relationships.
Osama Hamid indicated no relevant financial relationships.
Sushrut Trakroo indicated no relevant financial relationships.
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
M Housam Nanah indicated no relevant financial relationships.
Omar Massoud indicated no relevant financial relationships.
Ahmed Eltelbany, MD, MPH, Rama Nanah, MD, Osama Hamid, MD, MRCPI, Sushrut Trakroo, MD, Khaled Alsabbagh Alchirazi, MD, M Housam Nanah, MD, Omar Massoud, MD. A0575 - A Rare Case of Antiphospholipid Syndrome Presenting With Variceal Bleeding and Ascites Secondary to Portal Vein Thrombosis Without Liver Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
