Back

Poster Session C - Monday Afternoon
Category: Liver
C0609 - An Unusual Presentation of Seronegative Autoimmune Hepatitis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Gagan Verma, DO, MPH
Stony Brook University Hospital
Stony Brook, NY
Presenting Author(s)
Gagan Verma, DO, MPH, Adam Meyer, MD, Joseph Mizrahi, MD, Edward Sun, MD, MBA
Stony Brook University Hospital, Stony Brook, NY
Introduction: Seronegative autoimmune hepatitis presenting as acute liver failure is uncommon.
Case Description/Methods: A 74-year-old woman with past medical history of GERD and moderate Alzheimer’s dementia was noted to have transaminitis on routine outpatient labs (ALT 272, AST 183), which did not resolve over four months. Her only medications were calcium and famotidine. She took no supplements or substances. She presented to the hospital after recent repeat chemistries showed worsening transaminitis.
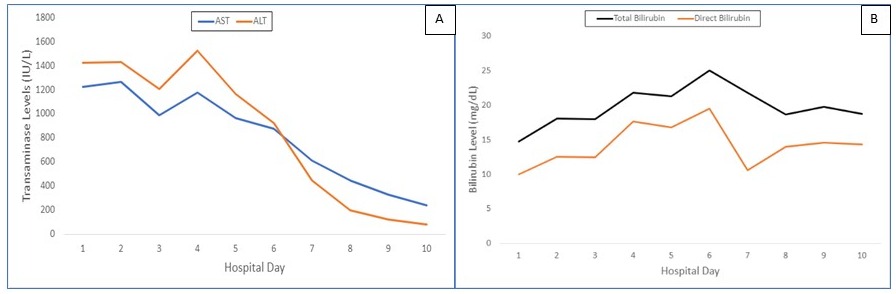
Upon admission, she appeared fatigued and jaundiced. Family noted she was unable to care for herself as usual. Initial labs revealed: total bilirubin 14.8 mg/dL, direct bilirubin 10.0 mg/dL, INR 1.7, AST / ALT 1428 and 1224 IU/L, Alk Phos 168 IU/L , Albumin 3.4 g/dL. Toxicology, immunologic serologies, including anti-smooth muscle antibodies (ASMA), and infectious testing were unremarkable. Immunoglobulin G was elevated (2700). CT of the abdomen and pelvis noted a small lesion in the pancreas and pancreatic and periportal adenopathy, and an enlarged gallbladder with sludge. She was admitted to medical oncology with a presumed diagnosis of pancreatic cancer. She could not complete MRI and underwent endoscopic ultrasound (EUS) on hospital day 4, which revealed normal pancreas and bile ducts. EUS-guided biopsy of the liver was done. On hospital day 6, she developed acute liver failure and methylprednisolone and N-acetylcysteine were started. Due to dementia, she was ineligible for liver transplant. On hospital day 8, pathology confirmed autoimmune hepatitis with bridging fibrosis. By hospital day 10, liver function improved (Figure 1 A-B); however, she developed fever and, despite broad-spectrum antibiotics, suffered from septic shock and expired on day 11.
Discussion: Fulminant-onset autoimmune hepatitis (AIH) with hepatic encephalopathy is rare, occurring in < 6% of patients with AIH. The frequency of seronegative autoimmune hepatitis in acute and severe AIH is further estimated to be ≤7%. This case illustrates the challenge in diagnosis, particularly when confounding factors are present. Our patient suffered from dementia and aphasia, which masked developing hepatic encephalopathy, and pancreatic cancer was initially suspected as the cause of her painless jaundice, which delayed steroid treatment. A high index of suspicion for AIH is needed in patients with liver failure of uncertain etiology, as early treatment with steroids may improve the clinical outcome.
Disclosures:
Gagan Verma, DO, MPH, Adam Meyer, MD, Joseph Mizrahi, MD, Edward Sun, MD, MBA. C0609 - An Unusual Presentation of Seronegative Autoimmune Hepatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Stony Brook University Hospital, Stony Brook, NY
Introduction: Seronegative autoimmune hepatitis presenting as acute liver failure is uncommon.
Case Description/Methods: A 74-year-old woman with past medical history of GERD and moderate Alzheimer’s dementia was noted to have transaminitis on routine outpatient labs (ALT 272, AST 183), which did not resolve over four months. Her only medications were calcium and famotidine. She took no supplements or substances. She presented to the hospital after recent repeat chemistries showed worsening transaminitis.
Upon admission, she appeared fatigued and jaundiced. Family noted she was unable to care for herself as usual. Initial labs revealed: total bilirubin 14.8 mg/dL, direct bilirubin 10.0 mg/dL, INR 1.7, AST / ALT 1428 and 1224 IU/L, Alk Phos 168 IU/L , Albumin 3.4 g/dL. Toxicology, immunologic serologies, including anti-smooth muscle antibodies (ASMA), and infectious testing were unremarkable. Immunoglobulin G was elevated (2700). CT of the abdomen and pelvis noted a small lesion in the pancreas and pancreatic and periportal adenopathy, and an enlarged gallbladder with sludge. She was admitted to medical oncology with a presumed diagnosis of pancreatic cancer. She could not complete MRI and underwent endoscopic ultrasound (EUS) on hospital day 4, which revealed normal pancreas and bile ducts. EUS-guided biopsy of the liver was done. On hospital day 6, she developed acute liver failure and methylprednisolone and N-acetylcysteine were started. Due to dementia, she was ineligible for liver transplant. On hospital day 8, pathology confirmed autoimmune hepatitis with bridging fibrosis. By hospital day 10, liver function improved (Figure 1 A-B); however, she developed fever and, despite broad-spectrum antibiotics, suffered from septic shock and expired on day 11.
Discussion: Fulminant-onset autoimmune hepatitis (AIH) with hepatic encephalopathy is rare, occurring in < 6% of patients with AIH. The frequency of seronegative autoimmune hepatitis in acute and severe AIH is further estimated to be ≤7%. This case illustrates the challenge in diagnosis, particularly when confounding factors are present. Our patient suffered from dementia and aphasia, which masked developing hepatic encephalopathy, and pancreatic cancer was initially suspected as the cause of her painless jaundice, which delayed steroid treatment. A high index of suspicion for AIH is needed in patients with liver failure of uncertain etiology, as early treatment with steroids may improve the clinical outcome.
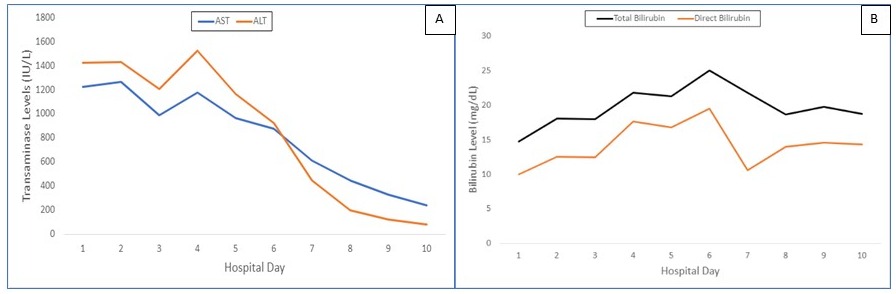
Figure: Figure 1 (A-B)
Disclosures:
Gagan Verma indicated no relevant financial relationships.
Adam Meyer indicated no relevant financial relationships.
Joseph Mizrahi indicated no relevant financial relationships.
Edward Sun indicated no relevant financial relationships.
Gagan Verma, DO, MPH, Adam Meyer, MD, Joseph Mizrahi, MD, Edward Sun, MD, MBA. C0609 - An Unusual Presentation of Seronegative Autoimmune Hepatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
