Back

Poster Session B - Monday Morning
Category: Liver
B0624 - Armillifer armillatus, Travel Token From Toga: Innumerable Asymptomatic Liver Calcifications
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Anastasia Novikov, MD
Elmhurst Hospital Center
Elmhurst, NY
Presenting Author(s)
Tracey O'Brien, MD1, Saphwat Eskaros, MD1, Anastasia Novikov, MD2
1Queens Hospital Center, Jamaica, NY; 2Elmhurst Hospital Center, Elmhurst, NY
Introduction: Armillifer armillatus found in tropical Africa, typical hosts are pythons,rodents presumed to be intermediate hosts. Accidental infection reported in humans stemming from consumption of infected snakes sold as the bushmeat. Most infections are asymptomatic, but there exist rare reports of debilitating and rarely fatal infections.
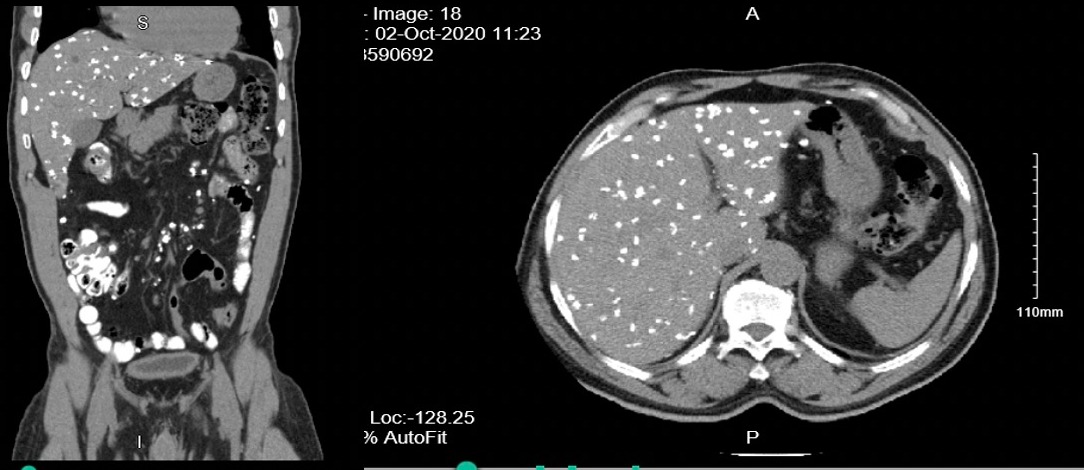
Case Description/Methods: 61 yo M with HTN, h/o malaria,chronic back pain presented for primary care visit. DX lumbar spine obtained and showed multiple calcifications,followed by CT abdomen pelvis with following findings: extensive subcentimeter calcifications throughout liver and mesentery. Laboratory data did not show LFT abnormality. CBC with elevated eosinophil count ranging 4.1-6.2%. Upon evaluation with EGD/colonoscopy, seven 5 to 10 mm submucosal polypoid lesions in the rectum, transverse colon,hepatic flexure, and cecum. One of the polypoid lesion was removed with a hot snare. Path showed completely calcified nodule in the submucosa. PAS stain failed to show any parasites, pathology, however, favoring infection such as parasite associated. Standard ova and parasite panel is negative for all organisms tested in the panel.
Discussion: The first documentation of human infection by Armifiller armilatus dates back to 1847,several cases were since documented with noted male predominance possibly attributed to more adventurous lifestyle and greater prevalence of certain activities. Most cases of Armillifer armillatus infestations are asymptomatic with only few with mild symptoms such as dry cough attributed to pneumonitis in a setting of parasitic infection. In patients with severe infestation, there could be associated pericarditis, pleuritis, acute abdominal conditions (intestinal obstruction,viscus perforation).These acute abdominal conditions have resulted in unnecessary laparotomy before true diagnosis was made. Close surveillance using abdominal ultrasound scan, liver function test and fecal occult blood test are advised in view of the radiologically confirmed severe hepatic affectation. Diagnosis usually is made incidentally as in our case when radiographic study obtained for unrelated reasons with findings of extensive crescentic calcific lesions in the lungs, peritoneum and liver. Some patients may have deranged LFTs. This is usually seen in those with severe liver affectation as noted by some authors. Our patient had normal liver function test parameters despite severe liver involvement. Liver biopsy is required as complementary investigation tool.
Disclosures:
Tracey O'Brien, MD1, Saphwat Eskaros, MD1, Anastasia Novikov, MD2. B0624 - Armillifer armillatus, Travel Token From Toga: Innumerable Asymptomatic Liver Calcifications, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Queens Hospital Center, Jamaica, NY; 2Elmhurst Hospital Center, Elmhurst, NY
Introduction: Armillifer armillatus found in tropical Africa, typical hosts are pythons,rodents presumed to be intermediate hosts. Accidental infection reported in humans stemming from consumption of infected snakes sold as the bushmeat. Most infections are asymptomatic, but there exist rare reports of debilitating and rarely fatal infections.
Case Description/Methods: 61 yo M with HTN, h/o malaria,chronic back pain presented for primary care visit. DX lumbar spine obtained and showed multiple calcifications,followed by CT abdomen pelvis with following findings: extensive subcentimeter calcifications throughout liver and mesentery. Laboratory data did not show LFT abnormality. CBC with elevated eosinophil count ranging 4.1-6.2%. Upon evaluation with EGD/colonoscopy, seven 5 to 10 mm submucosal polypoid lesions in the rectum, transverse colon,hepatic flexure, and cecum. One of the polypoid lesion was removed with a hot snare. Path showed completely calcified nodule in the submucosa. PAS stain failed to show any parasites, pathology, however, favoring infection such as parasite associated. Standard ova and parasite panel is negative for all organisms tested in the panel.
Discussion: The first documentation of human infection by Armifiller armilatus dates back to 1847,several cases were since documented with noted male predominance possibly attributed to more adventurous lifestyle and greater prevalence of certain activities. Most cases of Armillifer armillatus infestations are asymptomatic with only few with mild symptoms such as dry cough attributed to pneumonitis in a setting of parasitic infection. In patients with severe infestation, there could be associated pericarditis, pleuritis, acute abdominal conditions (intestinal obstruction,viscus perforation).These acute abdominal conditions have resulted in unnecessary laparotomy before true diagnosis was made. Close surveillance using abdominal ultrasound scan, liver function test and fecal occult blood test are advised in view of the radiologically confirmed severe hepatic affectation. Diagnosis usually is made incidentally as in our case when radiographic study obtained for unrelated reasons with findings of extensive crescentic calcific lesions in the lungs, peritoneum and liver. Some patients may have deranged LFTs. This is usually seen in those with severe liver affectation as noted by some authors. Our patient had normal liver function test parameters despite severe liver involvement. Liver biopsy is required as complementary investigation tool.
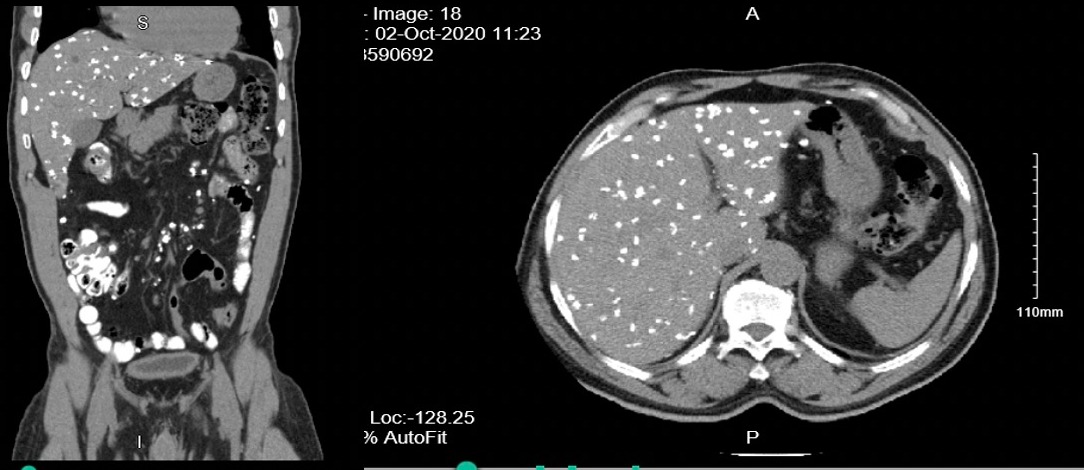
Figure: innumerable subcentimeter calcified liver inclusions
Disclosures:
Tracey O'Brien indicated no relevant financial relationships.
Saphwat Eskaros indicated no relevant financial relationships.
Anastasia Novikov indicated no relevant financial relationships.
Tracey O'Brien, MD1, Saphwat Eskaros, MD1, Anastasia Novikov, MD2. B0624 - Armillifer armillatus, Travel Token From Toga: Innumerable Asymptomatic Liver Calcifications, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
