Back

Poster Session C - Monday Afternoon
Category: Liver
C0611 - Plugging up the Leak After Transplant: Shunt-Induced Encephalopathy PARTO-ly Treated and Completed With CARTO
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
.jpeg.jpg)
Carl L. Kay, MD
Brooke Army Medical Center
JBSA Fort Sam Houston, TX
Presenting Author(s)
Carl L. Kay, MD1, Christian Horn, MD1, Omer Junaidi, MD2
1Brooke Army Medical Center, JBSA Fort Sam Houston, TX; 2Methodist Hospital Specialty and Transplant, San Antonio, TX
Introduction: Spontaneous portosystemic shunts (SPSS) are a common cause of recurrent hepatic encephalopathy (HE) in patients with cirrhosis. Liver transplant (LT) is the definitive treatment of end-stage liver disease and its complications, but SPSS may persist after LT. It is rare for SPSS to cause HE after LT; however, it is a treatable cause of encephalopathy.
Case Description/Methods: A 52-year-old female had an orthotopic liver transplantation for decompensated cirrhosis due to non-alcoholic steatohepatitis. Two months later, her post-transplant course began to be complicated by recurrent episodes of encephalopathy. She was diagnosed with HE after extensive unremarkable work-up – including metabolic, infectious, advanced brain imaging, electroencephalography, cerebrospinal fluid analysis, and neurology evaluation. The diagnosis was also supported by persistent hyperammonemia and improvement of sensorium with initiation of lactulose. In total, she had four episodes of overt HE requiring hospitalization.
She had a transjugular liver biopsy which revealed stage 1 fibrosis but no evidence of graft cirrhosis or rejection. She had normal graft synthetic function. CT scan of the abdomen 8 months after transplant demonstrated a large inferior mesenteric to left renal vein shunt measuring 16 mm in diameter. This was confirmed by transjugular mesenteric venogram and excluded portal vein thrombosis or stenosis. She underwent plug-assisted retrograde transvenous occlusion (PARTO) of the shunt using 22 mm vascular plug. Coil-assisted retrograde transvenous obliteration (CARTO) technique with two 6 mm interlocked coils were used to treat residual collaterals in order to complete a successful shunt closure. In six months of follow up, she has not had any further episodes of HE or required any lactulose.
Discussion: Post-LT encephalopathy has a broad differential and SPSS is a rare cause of HE - especially without graft cirrhosis. After excluding alternative etiologies, it is important to recognize that SPSS can be treated with embolization. Successfully treated patients can avoid a significant amount of morbidity associated with recurrent hospitalizations and ongoing pharmacologic management. We describe the second known case of combined PARTO/CARTO technique to treat post-LT SPSS-related HE. This is only the 9th identified case of post-LT SPSS closure for treatment of HE. Not only is shunt closure feasible, but it is also safe within the 1st year of transplantation without thrombosis or need for repeat embolization.

Disclosures:
Carl L. Kay, MD1, Christian Horn, MD1, Omer Junaidi, MD2. C0611 - Plugging up the Leak After Transplant: Shunt-Induced Encephalopathy PARTO-ly Treated and Completed With CARTO, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Brooke Army Medical Center, JBSA Fort Sam Houston, TX; 2Methodist Hospital Specialty and Transplant, San Antonio, TX
Introduction: Spontaneous portosystemic shunts (SPSS) are a common cause of recurrent hepatic encephalopathy (HE) in patients with cirrhosis. Liver transplant (LT) is the definitive treatment of end-stage liver disease and its complications, but SPSS may persist after LT. It is rare for SPSS to cause HE after LT; however, it is a treatable cause of encephalopathy.
Case Description/Methods: A 52-year-old female had an orthotopic liver transplantation for decompensated cirrhosis due to non-alcoholic steatohepatitis. Two months later, her post-transplant course began to be complicated by recurrent episodes of encephalopathy. She was diagnosed with HE after extensive unremarkable work-up – including metabolic, infectious, advanced brain imaging, electroencephalography, cerebrospinal fluid analysis, and neurology evaluation. The diagnosis was also supported by persistent hyperammonemia and improvement of sensorium with initiation of lactulose. In total, she had four episodes of overt HE requiring hospitalization.
She had a transjugular liver biopsy which revealed stage 1 fibrosis but no evidence of graft cirrhosis or rejection. She had normal graft synthetic function. CT scan of the abdomen 8 months after transplant demonstrated a large inferior mesenteric to left renal vein shunt measuring 16 mm in diameter. This was confirmed by transjugular mesenteric venogram and excluded portal vein thrombosis or stenosis. She underwent plug-assisted retrograde transvenous occlusion (PARTO) of the shunt using 22 mm vascular plug. Coil-assisted retrograde transvenous obliteration (CARTO) technique with two 6 mm interlocked coils were used to treat residual collaterals in order to complete a successful shunt closure. In six months of follow up, she has not had any further episodes of HE or required any lactulose.
Discussion: Post-LT encephalopathy has a broad differential and SPSS is a rare cause of HE - especially without graft cirrhosis. After excluding alternative etiologies, it is important to recognize that SPSS can be treated with embolization. Successfully treated patients can avoid a significant amount of morbidity associated with recurrent hospitalizations and ongoing pharmacologic management. We describe the second known case of combined PARTO/CARTO technique to treat post-LT SPSS-related HE. This is only the 9th identified case of post-LT SPSS closure for treatment of HE. Not only is shunt closure feasible, but it is also safe within the 1st year of transplantation without thrombosis or need for repeat embolization.

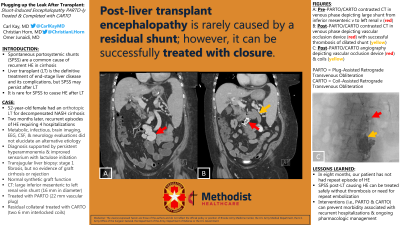
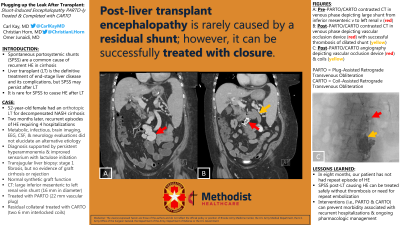
Figure: Figure 1A: Pre-PARTO/CARTO contrasted computed tomography (coronal view) in the venous phase depicting the large tortuous shunt from the inferior mesenteric vein to the left renal vein (red arrow);
Figure 1B: Post-PARTO/CARTO contrasted computed tomography (coronal view) in the venous phase depicting vascular occlusion device (red arrow) with successful thrombosis of the dilated shunt (yellow arrow);
Figure 1C: Post-PARTO/CARTO angiography depicting vascular occlusion device (red arrow) and coils (yellow arrow)
Figure 1B: Post-PARTO/CARTO contrasted computed tomography (coronal view) in the venous phase depicting vascular occlusion device (red arrow) with successful thrombosis of the dilated shunt (yellow arrow);
Figure 1C: Post-PARTO/CARTO angiography depicting vascular occlusion device (red arrow) and coils (yellow arrow)
Disclosures:
Carl Kay indicated no relevant financial relationships.
Christian Horn indicated no relevant financial relationships.
Omer Junaidi indicated no relevant financial relationships.
Carl L. Kay, MD1, Christian Horn, MD1, Omer Junaidi, MD2. C0611 - Plugging up the Leak After Transplant: Shunt-Induced Encephalopathy PARTO-ly Treated and Completed With CARTO, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
