Back
Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0012 - Early vs Delayed Minimally Invasive Intervention for Infected Pancreatic Necrosis – A Systematic Review and Meta-Analysis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Sami Ghazaleh, MD
University of Toledo
Toledo, OH
Presenting Author(s)
Sami Ghazaleh, MD1, Azizullah A. Beran, MD2, Wasef Sayeh, MD1, Justin Chuang, MD1, Amna Iqbal, MD1, Sudheer Dhoop, MD1, Mohammad Safi, MD1, Sabeen Sidiki, MD1, Yaseen Alastal, MD, MPH1, Ali Nawras, MD1
1University of Toledo, Toledo, OH; 2The University of Toledo, Toledo, OH
Introduction: Pancreatic necrosis complicates about 20% of acute pancreatitis cases, and 30-40% of those become infected. Current guidelines recommend that invasive intervention for pancreatic necrosis should be delayed to 4 or more weeks from disease onset. However, recent studies have challenged the optimal timing of intervention, especially with the advent of minimally invasive interventions.
Methods: We conducted a systematic review and meta-analysis of studies that early and delayed minimally invasive intervention for infected pancreatic necrosis. We performed a comprehensive search in the databases of PubMed/MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials from inception through April 11, 2022. We considered randomized controlled trials, cohort studies, case-control studies, and case series. We excluded abstracts, animal studies, case reports, reviews, editorials, and letters to editors. From each study, we collected the number of patients who underwent early and late interventions for infected pancreatic necrosis. Early intervention was defined as an intervention that was carried out within 4 weeks of acute pancreatitis onset, while delayed intervention was carried out after 4 weeks of acute pancreatitis onset. Outcomes were mortality, gastrointestinal fistula or perforation, bleeding, and length of hospital stay. The random-effects model was used to calculate the risk ratios (RR), mean differences (MD), and confidence intervals (CI). A p value < 0.05 was considered statistically significant. Heterogeneity was assessed using the Higgins I2 index.
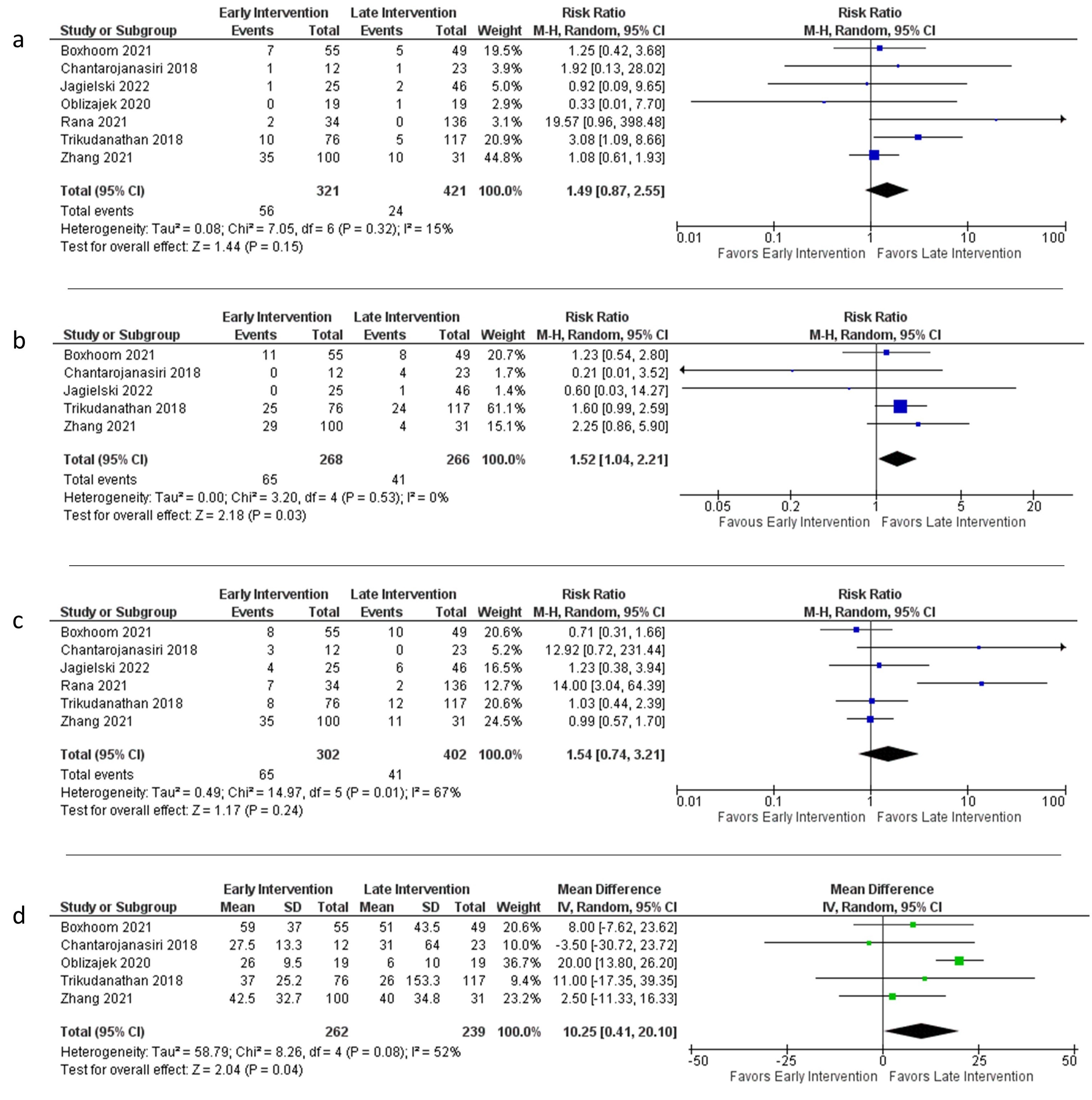
Results: Seven studies involving 742 patients were included in the meta-analysis. Timing of intervention had no statistically significant effect on mortality (RR 1.49, 95% CI 0.87 – 2.55, p = 0.15, I2 = 15%) or bleeding (RR 1.54, 95% CI 0.74 – 3.21, p = 0.24, I2 = 67%). However, early intervention was associated with a statistically significant higher risk of gastrointestinal fistula or perforation (RR 1.52, 95% CI 1.04 – 2.21, p = 0.03, I2 = 0%) and a longer hospital length of stay (MD 10.25 days, 95% CI 0.41 – 20.10, p = 0.04, I2 = 52%).
Discussion: Our meta-analysis demonstrated that the timing of intervention had no effect on mortality or bleeding in infected pancreatic necrosis. Early intervention resulted in a higher risk of gastrointestinal fistula or perforation and a longer length of hospital stay. Further randomized controlled trials are needed to confirm our findings.
Disclosures:
Sami Ghazaleh, MD1, Azizullah A. Beran, MD2, Wasef Sayeh, MD1, Justin Chuang, MD1, Amna Iqbal, MD1, Sudheer Dhoop, MD1, Mohammad Safi, MD1, Sabeen Sidiki, MD1, Yaseen Alastal, MD, MPH1, Ali Nawras, MD1. D0012 - Early vs Delayed Minimally Invasive Intervention for Infected Pancreatic Necrosis – A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Toledo, Toledo, OH; 2The University of Toledo, Toledo, OH
Introduction: Pancreatic necrosis complicates about 20% of acute pancreatitis cases, and 30-40% of those become infected. Current guidelines recommend that invasive intervention for pancreatic necrosis should be delayed to 4 or more weeks from disease onset. However, recent studies have challenged the optimal timing of intervention, especially with the advent of minimally invasive interventions.
Methods: We conducted a systematic review and meta-analysis of studies that early and delayed minimally invasive intervention for infected pancreatic necrosis. We performed a comprehensive search in the databases of PubMed/MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials from inception through April 11, 2022. We considered randomized controlled trials, cohort studies, case-control studies, and case series. We excluded abstracts, animal studies, case reports, reviews, editorials, and letters to editors. From each study, we collected the number of patients who underwent early and late interventions for infected pancreatic necrosis. Early intervention was defined as an intervention that was carried out within 4 weeks of acute pancreatitis onset, while delayed intervention was carried out after 4 weeks of acute pancreatitis onset. Outcomes were mortality, gastrointestinal fistula or perforation, bleeding, and length of hospital stay. The random-effects model was used to calculate the risk ratios (RR), mean differences (MD), and confidence intervals (CI). A p value < 0.05 was considered statistically significant. Heterogeneity was assessed using the Higgins I2 index.
Results: Seven studies involving 742 patients were included in the meta-analysis. Timing of intervention had no statistically significant effect on mortality (RR 1.49, 95% CI 0.87 – 2.55, p = 0.15, I2 = 15%) or bleeding (RR 1.54, 95% CI 0.74 – 3.21, p = 0.24, I2 = 67%). However, early intervention was associated with a statistically significant higher risk of gastrointestinal fistula or perforation (RR 1.52, 95% CI 1.04 – 2.21, p = 0.03, I2 = 0%) and a longer hospital length of stay (MD 10.25 days, 95% CI 0.41 – 20.10, p = 0.04, I2 = 52%).
Discussion: Our meta-analysis demonstrated that the timing of intervention had no effect on mortality or bleeding in infected pancreatic necrosis. Early intervention resulted in a higher risk of gastrointestinal fistula or perforation and a longer length of hospital stay. Further randomized controlled trials are needed to confirm our findings.
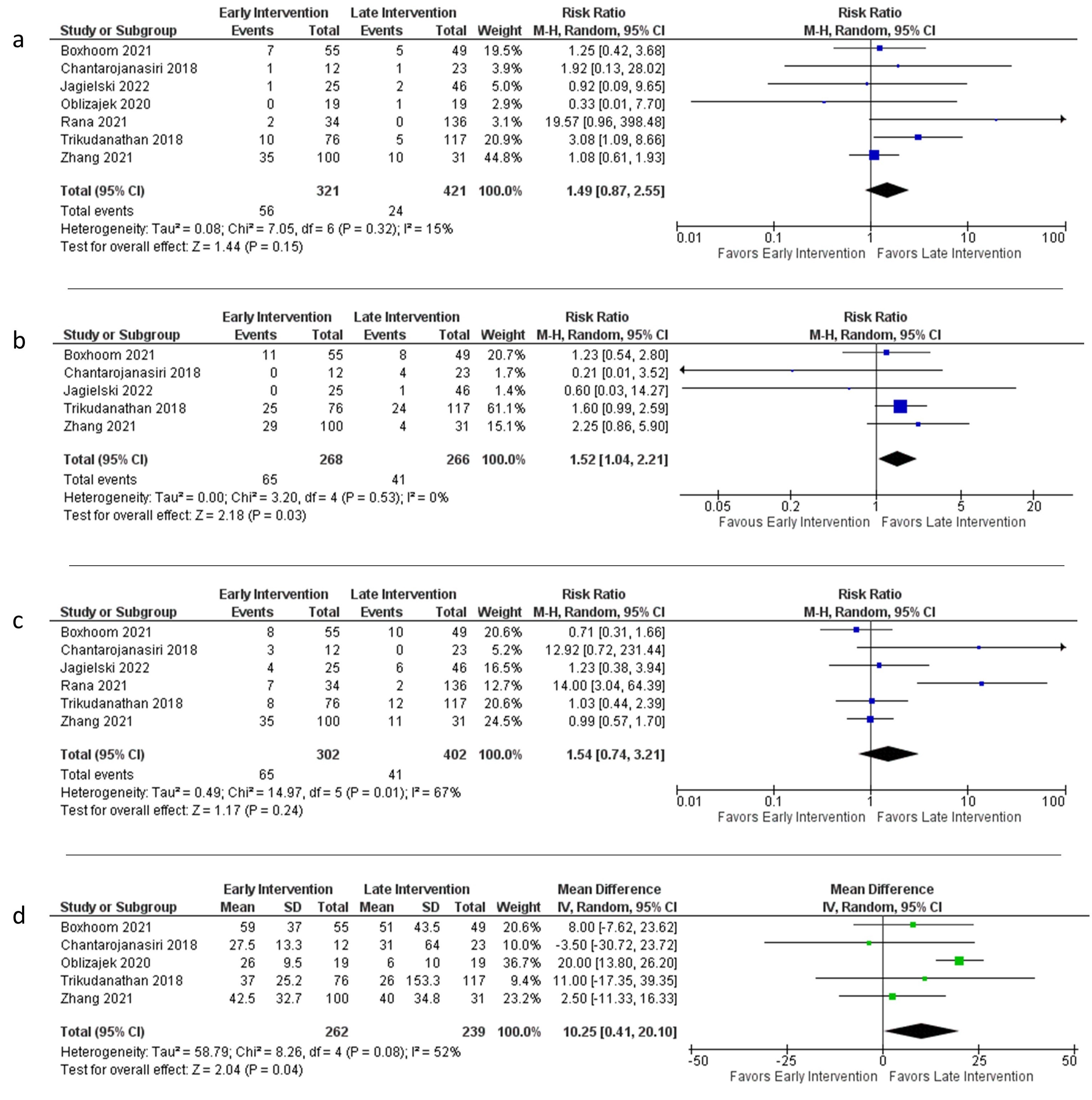
Figure: Forest plots comparing early and late intervention in terms of (a) mortality, (b) gastrointestinal fistula or perforation, (c) bleeding, and (d) length of hospital stay
Disclosures:
Sami Ghazaleh indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Wasef Sayeh indicated no relevant financial relationships.
Justin Chuang indicated no relevant financial relationships.
Amna Iqbal indicated no relevant financial relationships.
Sudheer Dhoop indicated no relevant financial relationships.
Mohammad Safi indicated no relevant financial relationships.
Sabeen Sidiki indicated no relevant financial relationships.
Yaseen Alastal indicated no relevant financial relationships.
Ali Nawras indicated no relevant financial relationships.
Sami Ghazaleh, MD1, Azizullah A. Beran, MD2, Wasef Sayeh, MD1, Justin Chuang, MD1, Amna Iqbal, MD1, Sudheer Dhoop, MD1, Mohammad Safi, MD1, Sabeen Sidiki, MD1, Yaseen Alastal, MD, MPH1, Ali Nawras, MD1. D0012 - Early vs Delayed Minimally Invasive Intervention for Infected Pancreatic Necrosis – A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

