Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0078 - Cholelithiasis Causing Asymptomatic Cholecystoenteric Fistula
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Ian Nora, MBBS, MPH
Sarasota Memorial Hospital
Sarasota, Florida
Presenting Author(s)
Ian Nora, MBBS, MPH1, Ricardo Villasmil, MD2, Charles j. Loewe, MD3
1Sarasota Memorial Hospital, Sarasota, FL; 2Florida State University College of Medicine at Sarasota Memorial Hospital, Sarasota, FL; 3FDHS/SCDD, Sarasota, FL
Introduction: Biliary fistulas are a rare complication of gallstones. Fistula formation can occur in a number of adjacent sites; even more rare complication is the formation of a cholecystocolonic fistula.
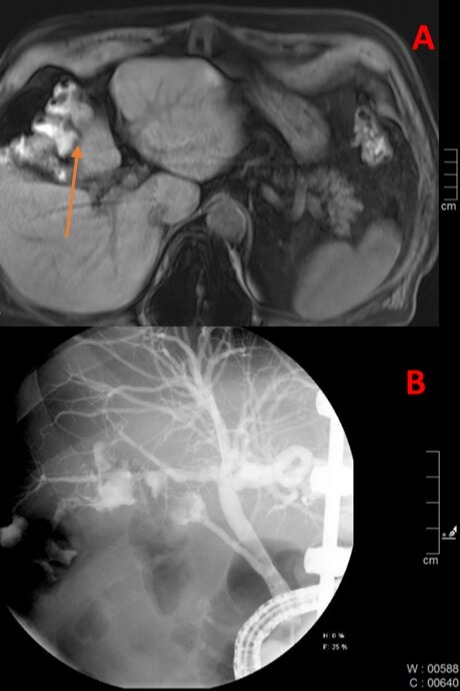
Case Description/Methods: A 74-year-old male who had recently undergone an extensive hospitalization secondary to inflammatory demyelinating polyneuropathy (IDP) and COVID-19 infection. During his hospitalization, he required ICU admission and mechanical ventilation with subsequent PEG tube placement. He was discharged to an inpatient rehabilitation facility when he developed worsening respiratory distress. Laboratory examinations were pertinent for ALT of 252, AST of 140 and ALP of 401 without hyperbilirubinemia. Blood cultures revealed Escherichia coli bacteremia. Given transaminitis and bacteremia, an MRCP was performed which demonstrated evidence absent space between gallbladder and hepatic flexure of the colon suggesting a CCF (figure 1a). An ERCP with sphincterotomy was performed which showed extravasation of contrast from the gallbladder into the colon at the hepatic flexure (figure 1b). He underwent cholecystectomy and fistula repair without any complications and gradual improvement in liver function test. He was discharged to a rehabilitation facility.
Discussion: Complications of gallstones are well established, which include the common bile duct obstruction, but also include the rare occurrences of acute cholangitis, malignancy, and fistula formation. CCF is a rare complication of gallstones which can occur in the stomach, duodenum, or colon with a variable clinical presentation. Complications from an undiagnosed fistula can be life threatening including colon perforation and fecal peritonitis.
This case highlights the diagnostic challenge and the high degree of clinical suspicion involved in establishing the diagnosis of CCF in patient without abdominal symptoms suggestive of gallbladder disease. We hypothesize that stone formation resulting in the development of the fistula may be secondary to the underlying history of IDP and subsequent immobility. Although rare, CCF should be considered in patients presenting with unexplained pneumobilia and bacteremia. A timely diagnosis should be made to proceed with immediate treatment including cholecystectomy and fistula closure to prevent fatal complications.
Disclosures:
Ian Nora, MBBS, MPH1, Ricardo Villasmil, MD2, Charles j. Loewe, MD3. A0078 - Cholelithiasis Causing Asymptomatic Cholecystoenteric Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Sarasota Memorial Hospital, Sarasota, FL; 2Florida State University College of Medicine at Sarasota Memorial Hospital, Sarasota, FL; 3FDHS/SCDD, Sarasota, FL
Introduction: Biliary fistulas are a rare complication of gallstones. Fistula formation can occur in a number of adjacent sites; even more rare complication is the formation of a cholecystocolonic fistula.
Case Description/Methods: A 74-year-old male who had recently undergone an extensive hospitalization secondary to inflammatory demyelinating polyneuropathy (IDP) and COVID-19 infection. During his hospitalization, he required ICU admission and mechanical ventilation with subsequent PEG tube placement. He was discharged to an inpatient rehabilitation facility when he developed worsening respiratory distress. Laboratory examinations were pertinent for ALT of 252, AST of 140 and ALP of 401 without hyperbilirubinemia. Blood cultures revealed Escherichia coli bacteremia. Given transaminitis and bacteremia, an MRCP was performed which demonstrated evidence absent space between gallbladder and hepatic flexure of the colon suggesting a CCF (figure 1a). An ERCP with sphincterotomy was performed which showed extravasation of contrast from the gallbladder into the colon at the hepatic flexure (figure 1b). He underwent cholecystectomy and fistula repair without any complications and gradual improvement in liver function test. He was discharged to a rehabilitation facility.
Discussion: Complications of gallstones are well established, which include the common bile duct obstruction, but also include the rare occurrences of acute cholangitis, malignancy, and fistula formation. CCF is a rare complication of gallstones which can occur in the stomach, duodenum, or colon with a variable clinical presentation. Complications from an undiagnosed fistula can be life threatening including colon perforation and fecal peritonitis.
This case highlights the diagnostic challenge and the high degree of clinical suspicion involved in establishing the diagnosis of CCF in patient without abdominal symptoms suggestive of gallbladder disease. We hypothesize that stone formation resulting in the development of the fistula may be secondary to the underlying history of IDP and subsequent immobility. Although rare, CCF should be considered in patients presenting with unexplained pneumobilia and bacteremia. A timely diagnosis should be made to proceed with immediate treatment including cholecystectomy and fistula closure to prevent fatal complications.
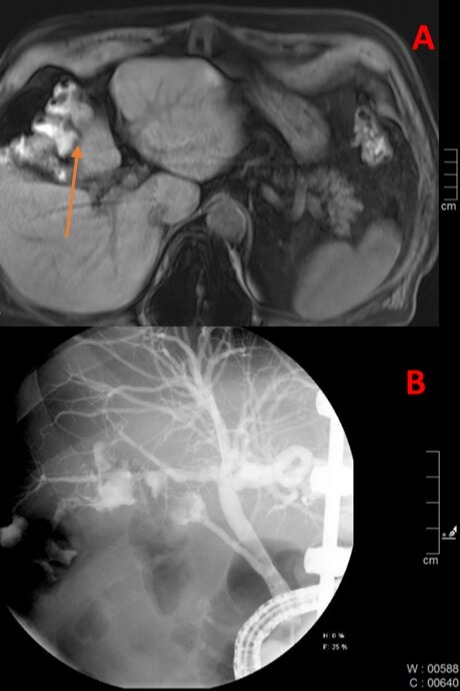
Figure: Figure 1: MRCP imaging of colon abutment with gallbladder (A) and ERCP cholangiogram showing extravasation of contrast into the hepatic flexure of the colon (B).
Disclosures:
Ian Nora indicated no relevant financial relationships.
Ricardo Villasmil indicated no relevant financial relationships.
Charles Loewe indicated no relevant financial relationships.
Ian Nora, MBBS, MPH1, Ricardo Villasmil, MD2, Charles j. Loewe, MD3. A0078 - Cholelithiasis Causing Asymptomatic Cholecystoenteric Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

