Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0052 - A Rare Case of Acute Necrotizing Pancreatitis Infected With Prevotella Species
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Cindy Traboulsi, MD
University of Pittsburgh Medical Center
Pittsburgh, PA
Presenting Author(s)
Cindy Traboulsi, MD, Nikola Gligorijevic, MD
University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Acute pancreatitis is one of the leading causes of GI-related hospitalizations in the USA. Around 20% of these cases are characterized as severe, leading to complications including necrotizing pancreatitis.1 Enterococci are the most-commonly isolated species in infected pancreatic necrosis followed by Escherichia coli, with anaerobic bacteria being more rarely involved.2 We present a rare case of acute necrotizing pancreatitis infected with Prevotella species in a young patient.
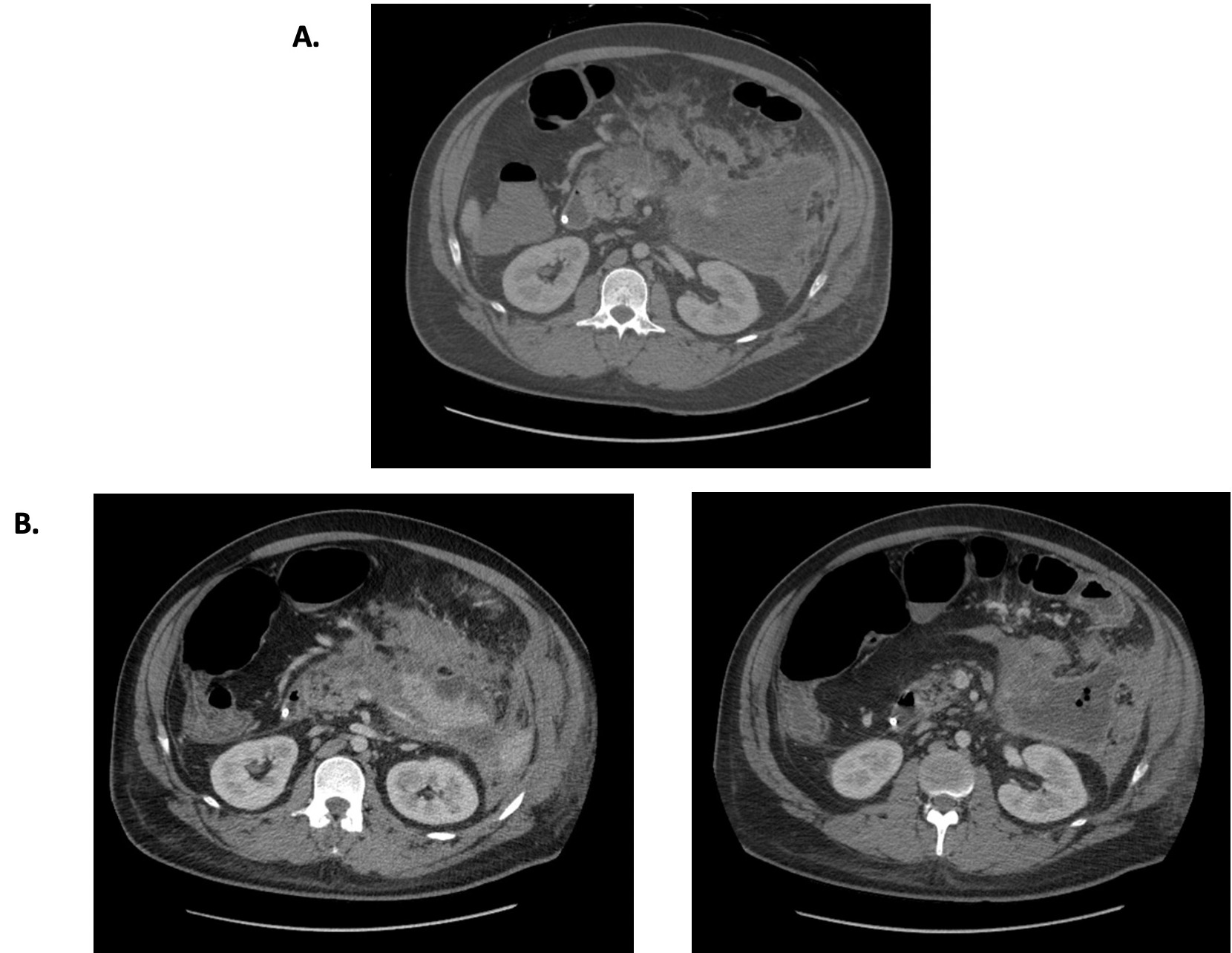
Case Description/Methods: 28-year-old man with ADHD and hypertension presented with acute epigastric pain radiating to the left. He was found to have a lipase level of 3897U/L, a triglyceride level of 2716mg/dL, in addition to acute interstitial pancreatitis with extensive peri-pancreatic inflammation on CT scan. He was admitted for pain control, IV fluids and insulin. During his stay, he also received plasma exchange for the treatment of hypertriglyceridemia and was discharged upon improvement of symptoms. He represented with abdominal pain and was found to have pancreatic walled-off necrosis with gas concerning for superimposed infection with gastric outlet and colonic obstruction (Figure). A percutaneous drain was placed; his course was complicated by sepsis and broad spectrum antibiotics were initiated. Drain fluid cultures grew moderate Staphylococcus aureus and Streptococcus intermedius, heavy Prevotella buccae, Prevotella denticola and Fusobacterium. Hospital course was further complicated by worsening abdominal pain and distention. Repeat CT revealed increasing colonic and small bowel dilatation due to stricture in descending colon. Gastroview enema demonstrated probable fistula tract. He underwent percutaneous endoscopic gastrostomy tube placement and creation of a loop transverse colostomy. Post-operatively, patient was transitioned to oral antibiotics for additional four weeks with outpatient follow-up.
Discussion: Acute necrotizing pancreatitis, especially if infected, is associated with poor outcomes. We highlight a rare case of hypertriglyceridemia-induced pancreatitis complicated by necrotizing infection with heavy Prevotella species. We demonstrate the importance of early suspicion of complicated acute pancreatitis and the need for early intervention to prevent hospital re-admission and improve the morbidity and mortality associated with infected pancreatic necrosis.
1. Al Mofleh,IA. World J of Gastroenterology.2008;14(5):675-684. 2. Dionigi R,et al.Surg Infect(larchmt).2006;7Suppl2:S49-52.
Disclosures:
Cindy Traboulsi, MD, Nikola Gligorijevic, MD. D0052 - A Rare Case of Acute Necrotizing Pancreatitis Infected With Prevotella Species, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Acute pancreatitis is one of the leading causes of GI-related hospitalizations in the USA. Around 20% of these cases are characterized as severe, leading to complications including necrotizing pancreatitis.1 Enterococci are the most-commonly isolated species in infected pancreatic necrosis followed by Escherichia coli, with anaerobic bacteria being more rarely involved.2 We present a rare case of acute necrotizing pancreatitis infected with Prevotella species in a young patient.
Case Description/Methods: 28-year-old man with ADHD and hypertension presented with acute epigastric pain radiating to the left. He was found to have a lipase level of 3897U/L, a triglyceride level of 2716mg/dL, in addition to acute interstitial pancreatitis with extensive peri-pancreatic inflammation on CT scan. He was admitted for pain control, IV fluids and insulin. During his stay, he also received plasma exchange for the treatment of hypertriglyceridemia and was discharged upon improvement of symptoms. He represented with abdominal pain and was found to have pancreatic walled-off necrosis with gas concerning for superimposed infection with gastric outlet and colonic obstruction (Figure). A percutaneous drain was placed; his course was complicated by sepsis and broad spectrum antibiotics were initiated. Drain fluid cultures grew moderate Staphylococcus aureus and Streptococcus intermedius, heavy Prevotella buccae, Prevotella denticola and Fusobacterium. Hospital course was further complicated by worsening abdominal pain and distention. Repeat CT revealed increasing colonic and small bowel dilatation due to stricture in descending colon. Gastroview enema demonstrated probable fistula tract. He underwent percutaneous endoscopic gastrostomy tube placement and creation of a loop transverse colostomy. Post-operatively, patient was transitioned to oral antibiotics for additional four weeks with outpatient follow-up.
Discussion: Acute necrotizing pancreatitis, especially if infected, is associated with poor outcomes. We highlight a rare case of hypertriglyceridemia-induced pancreatitis complicated by necrotizing infection with heavy Prevotella species. We demonstrate the importance of early suspicion of complicated acute pancreatitis and the need for early intervention to prevent hospital re-admission and improve the morbidity and mortality associated with infected pancreatic necrosis.
1. Al Mofleh,IA. World J of Gastroenterology.2008;14(5):675-684. 2. Dionigi R,et al.Surg Infect(larchmt).2006;7Suppl2:S49-52.
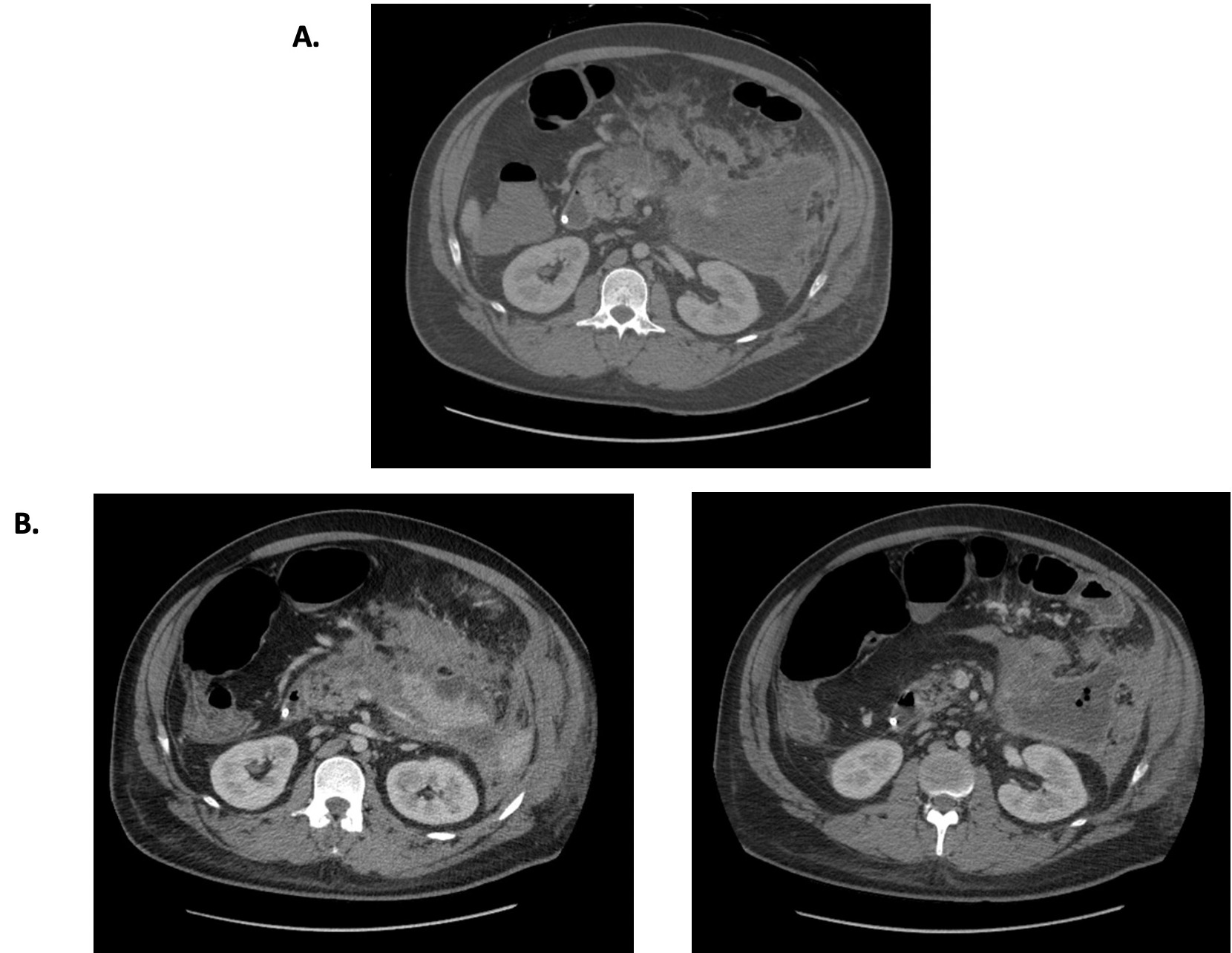
Figure: A. Initial CT showing necrotizing pancreatitis with large evolving peri-pancreatic walled off necrosis. B. Follow up CT showing large evolving peri-pancreatic walled off necrosis with evidence of new gas locules within the collection
Disclosures:
Cindy Traboulsi indicated no relevant financial relationships.
Nikola Gligorijevic indicated no relevant financial relationships.
Cindy Traboulsi, MD, Nikola Gligorijevic, MD. D0052 - A Rare Case of Acute Necrotizing Pancreatitis Infected With Prevotella Species, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
