Back

Poster Session B - Monday Morning
Category: IBD
B0429 - From Shortness of Breath to Bowel Unrest: COVID-19-Induced Ulcerative Colitis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Neil Patel, DO
Lehigh Valley Health Network
Allentown, PA
Presenting Author(s)
Neil Patel, DO1, Henry Lam, DO1, Olga Vitorsky, DO1, Aaron Mendelson, MD2
1Lehigh Valley Health Network, Allentown, PA; 2Eastern Pennsylvania Gastroenterology and Liver Specialists, Allentown, PA
Introduction: COVID-19 is recognized for its respiratory complications, but it can also cause extrapulmonary manifestations such as gastrointestinal complaints. Usually, GI manifestations are transient and rarely progress to chronic disease. We highlight a rare case of newly diagnosed ulcerative colitis triggered by COVID-19 infection.
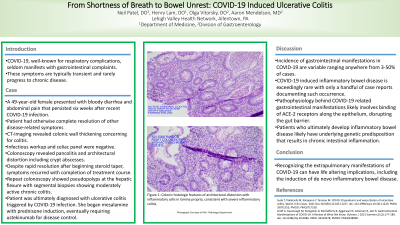
Case Description/Methods: A 49-year-old female with history of GERD presented with bloody diarrhea and abdominal pain that persisted six weeks after recent COVID-19 infection with otherwise complete resolution of other disease related symptoms. CT abdomen/pelvis showed colonic wall thickening from the hepatic flexure to the rectum concerning for colitis. Labs were significant for leukocytosis 13,600/microliter with elevated CRP 39.1 mg/L. Infectious workup and celiac panel were negative. Colonoscopy was performed and revealed pancolitis with pathology showing architectural distortion with crypt abscesses and chronic inflammatory cells in lamina propria. She was started on a steroid taper with rapid resolution of symptoms for presumed COVID-induced colitis. Unfortunately, upon completion of the taper, her symptoms recurred. Repeat labs showed CRP 8.7 mg/L with imaging negative for colitis. Repeat colonoscopy showed pseudopolyps at the hepatic flexure with segmental biopsies showing moderately active chronic colitis in the right colon. Patient was ultimately diagnosed with ulcerative colitis triggered by COVID-19 infection. She was started on Mesalamine with Prednisone induction eventually requiring Ustekinumab for disease control.
Discussion: Incidence of gastrointestinal manifestations in COVID-19 are variable ranging anywhere from 3-50% of cases. However, COVID-19 induced inflammatory bowel disease is exceedingly rare with only a handful of case reports documenting such occurrence. While not completely understood, the pathophysiology behind COVID-19 related gastrointestinal manifestations likely involves binding of ACE-2 receptors along the epithelium, disrupting the gut barrier. In most patients this disruption is self-resolving; however, patients who develop inflammatory bowel disease likely have underlying genetic predisposition that results in chronic intestinal inflammation. Our case demonstrates the importance of recognizing the extrapulmonary manifestations of COVID-19 which can have life altering implications as seen in our patient.
Disclosures:
Neil Patel, DO1, Henry Lam, DO1, Olga Vitorsky, DO1, Aaron Mendelson, MD2. B0429 - From Shortness of Breath to Bowel Unrest: COVID-19-Induced Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Lehigh Valley Health Network, Allentown, PA; 2Eastern Pennsylvania Gastroenterology and Liver Specialists, Allentown, PA
Introduction: COVID-19 is recognized for its respiratory complications, but it can also cause extrapulmonary manifestations such as gastrointestinal complaints. Usually, GI manifestations are transient and rarely progress to chronic disease. We highlight a rare case of newly diagnosed ulcerative colitis triggered by COVID-19 infection.
Case Description/Methods: A 49-year-old female with history of GERD presented with bloody diarrhea and abdominal pain that persisted six weeks after recent COVID-19 infection with otherwise complete resolution of other disease related symptoms. CT abdomen/pelvis showed colonic wall thickening from the hepatic flexure to the rectum concerning for colitis. Labs were significant for leukocytosis 13,600/microliter with elevated CRP 39.1 mg/L. Infectious workup and celiac panel were negative. Colonoscopy was performed and revealed pancolitis with pathology showing architectural distortion with crypt abscesses and chronic inflammatory cells in lamina propria. She was started on a steroid taper with rapid resolution of symptoms for presumed COVID-induced colitis. Unfortunately, upon completion of the taper, her symptoms recurred. Repeat labs showed CRP 8.7 mg/L with imaging negative for colitis. Repeat colonoscopy showed pseudopolyps at the hepatic flexure with segmental biopsies showing moderately active chronic colitis in the right colon. Patient was ultimately diagnosed with ulcerative colitis triggered by COVID-19 infection. She was started on Mesalamine with Prednisone induction eventually requiring Ustekinumab for disease control.
Discussion: Incidence of gastrointestinal manifestations in COVID-19 are variable ranging anywhere from 3-50% of cases. However, COVID-19 induced inflammatory bowel disease is exceedingly rare with only a handful of case reports documenting such occurrence. While not completely understood, the pathophysiology behind COVID-19 related gastrointestinal manifestations likely involves binding of ACE-2 receptors along the epithelium, disrupting the gut barrier. In most patients this disruption is self-resolving; however, patients who develop inflammatory bowel disease likely have underlying genetic predisposition that results in chronic intestinal inflammation. Our case demonstrates the importance of recognizing the extrapulmonary manifestations of COVID-19 which can have life altering implications as seen in our patient.
Disclosures:
Neil Patel indicated no relevant financial relationships.
Henry Lam indicated no relevant financial relationships.
Olga Vitorsky indicated no relevant financial relationships.
Aaron Mendelson indicated no relevant financial relationships.
Neil Patel, DO1, Henry Lam, DO1, Olga Vitorsky, DO1, Aaron Mendelson, MD2. B0429 - From Shortness of Breath to Bowel Unrest: COVID-19-Induced Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
