Back

Poster Session C - Monday Afternoon
Category: Liver
C0582 - Sickle Cell Hepatopathy in a Young Patient With Markedly Elevated Bilirubin
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Alexander Garcia, DO
Cooper Medical School at Rowan University, Cooper University Hospital
Camden, NJ
Presenting Author(s)
Alexander Garcia, DO1, Andrew Alabd, MD2, Upasana Joneja, MD2, Manav Bandlamudi, MD2
1Cooper Medical School at Rowan University, Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Camden, NJ
Introduction: The vaso-occlusive events that characterize a sickle cell pain crisis are known to affect multiple organ systems. Sickling in the hepatic sinusoids leads to ischemia, cholestasis, and sequestration, which collectively contribute to acute liver dysfunction often referred to as sickle cell hepatopathy (SCH). As one of the rarer complications of sickle cell disease (SCD) SCH may go under-recognized. Here we present a case of acute sickle cell hepatic crisis, a subset of SCH, with the aim of increasing the available literature on this important topic.
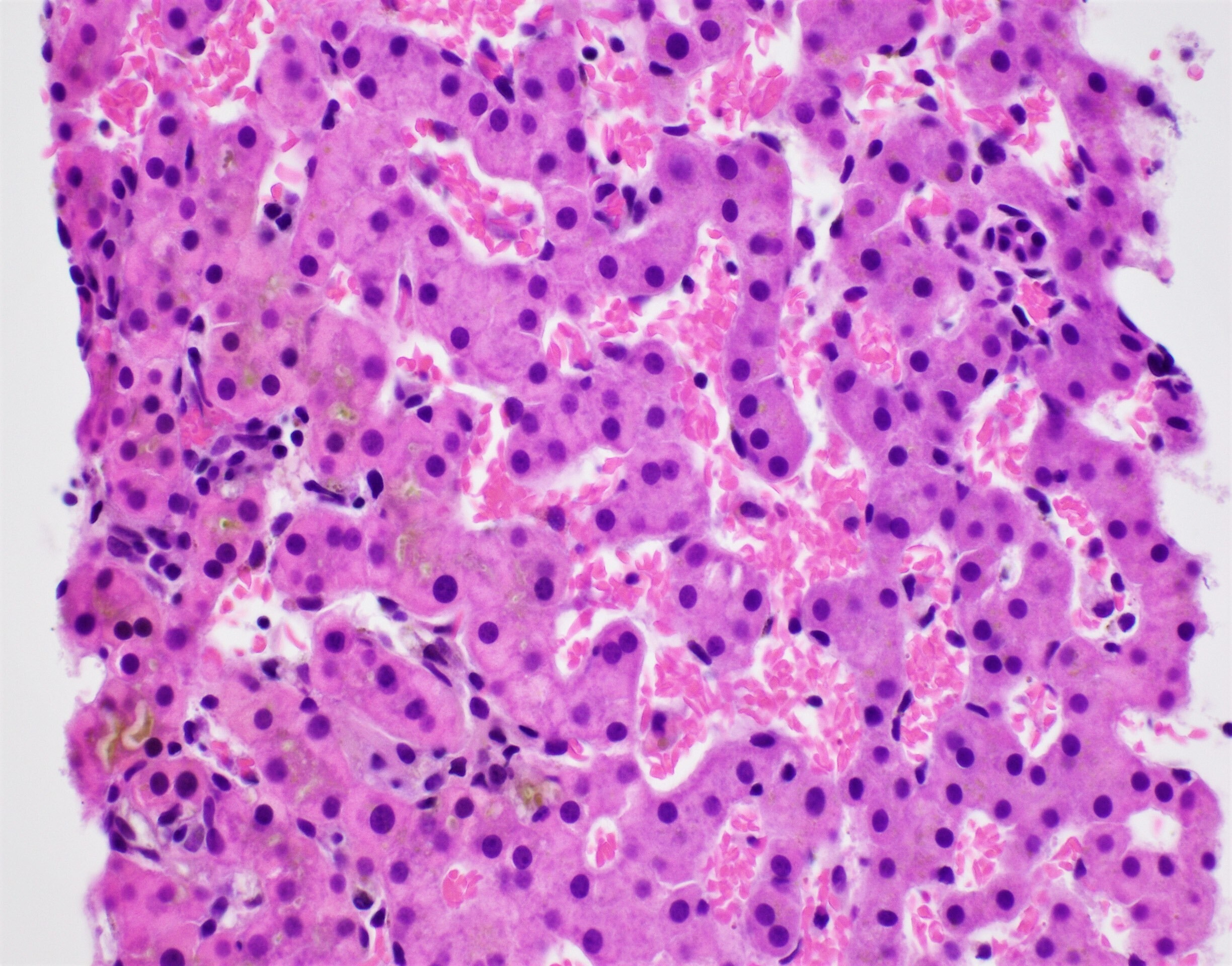
Case Description/Methods: A 20-year-old male with a history of sickle cell disease (SCD) presented for evaluation of right upper quadrant abdominal pain. Vitals signs were normal and physical examination was notable for jaundice and right upper quadrant abdominal tenderness. Labs revealed mildly elevated liver enzymes and elevated direct bilirubin of 34 mg/dL. Abdominal sonography revealed findings suggestive of hepatitis and common bile duct dilation, with suggestion of gallbladder wall thickening. MRCP showed mild intrahepatic and extrahepatic bile duct dilation, as well as splenic hemosiderosis. The common bile duct was 0.9 cm in diameter. Hepatitis A, B, C, as well as HIV, CMV, and herpes screening tests were nonreactive. An ultrasound-guided liver biopsy then revealed features of an acute sickle cell hepatic crisis, including distended sinusoids with erythrocyte sludging. With two days of symptomatic treatment alone, the patient had improvement in his direct bilirubin to 7 mg/dL and was discharged after complete resolution of his symptoms.
Discussion: Acute sickle cell hepatic crisis (ASCHC), a subset of sickle cell hepatopathy (SCH), is often difficult to diagnose for a multitude of reasons including vague presenting symptoms and clinician unfamiliarity with the disease. While treatment guidelines are lacking with regards to the specific treatment for ASCHC, it is worth noting that in our case clinical and assay improvement was seen after several days of symptomatic treatment alone. Although not present in our case, ASCHC has the potential to be concurrent with a more severe form of the disease known as sickle cell intrahepatic cholestasis (SCIC), which if untreated can be fatal. Both ASCHC and SCIC can present with jaundice, as in our patient, but only SCIC progresses to organ failure. As more cases are described, the optimal treatment modalities for these rarer complications of sickle cell disease will only increase.
Disclosures:
Alexander Garcia, DO1, Andrew Alabd, MD2, Upasana Joneja, MD2, Manav Bandlamudi, MD2. C0582 - Sickle Cell Hepatopathy in a Young Patient With Markedly Elevated Bilirubin, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Cooper Medical School at Rowan University, Cooper University Hospital, Camden, NJ; 2Cooper University Hospital, Camden, NJ
Introduction: The vaso-occlusive events that characterize a sickle cell pain crisis are known to affect multiple organ systems. Sickling in the hepatic sinusoids leads to ischemia, cholestasis, and sequestration, which collectively contribute to acute liver dysfunction often referred to as sickle cell hepatopathy (SCH). As one of the rarer complications of sickle cell disease (SCD) SCH may go under-recognized. Here we present a case of acute sickle cell hepatic crisis, a subset of SCH, with the aim of increasing the available literature on this important topic.
Case Description/Methods: A 20-year-old male with a history of sickle cell disease (SCD) presented for evaluation of right upper quadrant abdominal pain. Vitals signs were normal and physical examination was notable for jaundice and right upper quadrant abdominal tenderness. Labs revealed mildly elevated liver enzymes and elevated direct bilirubin of 34 mg/dL. Abdominal sonography revealed findings suggestive of hepatitis and common bile duct dilation, with suggestion of gallbladder wall thickening. MRCP showed mild intrahepatic and extrahepatic bile duct dilation, as well as splenic hemosiderosis. The common bile duct was 0.9 cm in diameter. Hepatitis A, B, C, as well as HIV, CMV, and herpes screening tests were nonreactive. An ultrasound-guided liver biopsy then revealed features of an acute sickle cell hepatic crisis, including distended sinusoids with erythrocyte sludging. With two days of symptomatic treatment alone, the patient had improvement in his direct bilirubin to 7 mg/dL and was discharged after complete resolution of his symptoms.
Discussion: Acute sickle cell hepatic crisis (ASCHC), a subset of sickle cell hepatopathy (SCH), is often difficult to diagnose for a multitude of reasons including vague presenting symptoms and clinician unfamiliarity with the disease. While treatment guidelines are lacking with regards to the specific treatment for ASCHC, it is worth noting that in our case clinical and assay improvement was seen after several days of symptomatic treatment alone. Although not present in our case, ASCHC has the potential to be concurrent with a more severe form of the disease known as sickle cell intrahepatic cholestasis (SCIC), which if untreated can be fatal. Both ASCHC and SCIC can present with jaundice, as in our patient, but only SCIC progresses to organ failure. As more cases are described, the optimal treatment modalities for these rarer complications of sickle cell disease will only increase.
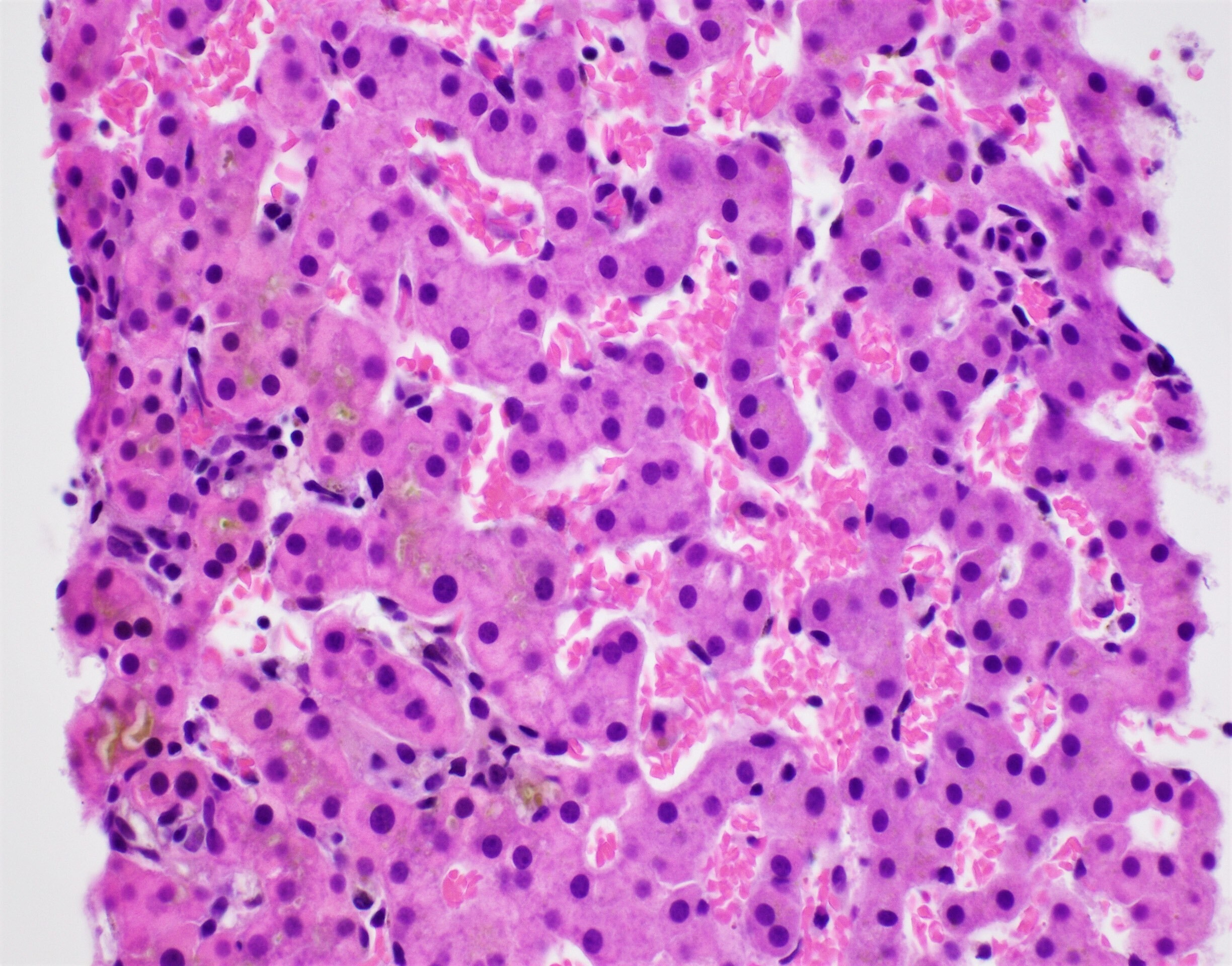
Figure: Liver parenchyma with dilated sinusoids, readily visualized sickled red blood cells (right side of the image) and canalicular cholestasis (brown pigment on the left side of the image).
Disclosures:
Alexander Garcia indicated no relevant financial relationships.
Andrew Alabd indicated no relevant financial relationships.
Upasana Joneja indicated no relevant financial relationships.
Manav Bandlamudi indicated no relevant financial relationships.
Alexander Garcia, DO1, Andrew Alabd, MD2, Upasana Joneja, MD2, Manav Bandlamudi, MD2. C0582 - Sickle Cell Hepatopathy in a Young Patient With Markedly Elevated Bilirubin, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
