Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0231 - Esophageal Stricture Recalcitrant to Repeated Dilation in Complex Rheumatological and Bullous Disease
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Caroline Olson, MD
Mayo Clinic Florida
Jacksonville, Florida
Presenting Author(s)
Caroline Olson, MD, Haily Vora, MD, MPH, Paul Kröner, MD, MS, Maoyin Pang, MD, PhD
Mayo Clinic Florida, Jacksonville, FL
Introduction: Many rheumatological diseases have been well characterized to affect the esophagus. Esophageal involvement in autoimmune bullous disease is rare and almost always occurs with severe cutaneous symptoms. We report a case of severe esophageal strictures recalcitrant to repeated dilatation in a patient with complex rheumatological disease and isolated esophageal bullous disease.
Case Description/Methods: A 50 year old female presented with complete inability to tolerate oral intake for several weeks. Past history included Sjogren's syndrome and esophageal strictures with many previous dilatations. Physical exam findings were relevant for poor skin turgor, dry mucous membranes, and skin hyperpigmentation on her hands and forearms. Laboratory studies showed hypokalemia, hypoalbuminemia, and anemia. The patient was admitted.
Her esophagram and esophagogastroduodenoscopy (EGD) showed a proximal esophageal stricture which was dilated using a push style dilator to 14mm. The stricture recurred, requiring repeated dilatation and placement of a percutaneous gastrojejunostomy. Once oral intake was tolerated, she was discharged with outpatient follow-up.
Outpatient rheumatological workup showed antibodies to ANA, RNP, SSA, CCP, and Smith indicating mixed connective tissue disease with features of systemic lupus erythematosus, rheumatoid arthritis, and scleroderma. She required multiple dilatations over several months and was started on mycophenolate mofetil with some clinical improvement.
The dysphagia recurred two months later and EGD showed and esophageal stricture measuring 7mm requiring a neonatal upper gastroscope to facilitate balloon dilatation. Biopsies examined for immunofluorescence showed continuous linear deposition along the basement membrane zone for IgG and C3, consistent with atypical esophageal bullous systemic lupus erythematosus or atypical esophageal bullous pemphigoid. The patient declined systemic steroids. Her mycophenolate mofetil dose was increased and she received weekly dilatations to prevent Koebnerization and allow time for medical therapy effect. After three months of treatment, she had symptom improvement.
Discussion: In patients with systemic immune mediated disorders including rheumatological disease, bullous diseases can be considered as a cause of esophageal stricture. Bullous disease with esophageal involvement can be difficult to treat, especially in this patient who declined corticosteroids. A combination approach using both immune suppression and dilatation was effective.
Disclosures:
Caroline Olson, MD, Haily Vora, MD, MPH, Paul Kröner, MD, MS, Maoyin Pang, MD, PhD. D0231 - Esophageal Stricture Recalcitrant to Repeated Dilation in Complex Rheumatological and Bullous Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Mayo Clinic Florida, Jacksonville, FL
Introduction: Many rheumatological diseases have been well characterized to affect the esophagus. Esophageal involvement in autoimmune bullous disease is rare and almost always occurs with severe cutaneous symptoms. We report a case of severe esophageal strictures recalcitrant to repeated dilatation in a patient with complex rheumatological disease and isolated esophageal bullous disease.
Case Description/Methods: A 50 year old female presented with complete inability to tolerate oral intake for several weeks. Past history included Sjogren's syndrome and esophageal strictures with many previous dilatations. Physical exam findings were relevant for poor skin turgor, dry mucous membranes, and skin hyperpigmentation on her hands and forearms. Laboratory studies showed hypokalemia, hypoalbuminemia, and anemia. The patient was admitted.
Her esophagram and esophagogastroduodenoscopy (EGD) showed a proximal esophageal stricture which was dilated using a push style dilator to 14mm. The stricture recurred, requiring repeated dilatation and placement of a percutaneous gastrojejunostomy. Once oral intake was tolerated, she was discharged with outpatient follow-up.
Outpatient rheumatological workup showed antibodies to ANA, RNP, SSA, CCP, and Smith indicating mixed connective tissue disease with features of systemic lupus erythematosus, rheumatoid arthritis, and scleroderma. She required multiple dilatations over several months and was started on mycophenolate mofetil with some clinical improvement.
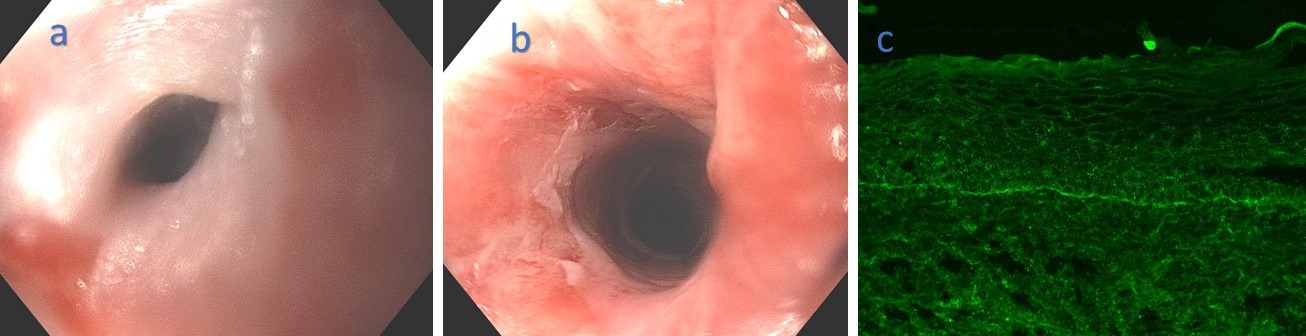
The dysphagia recurred two months later and EGD showed and esophageal stricture measuring 7mm requiring a neonatal upper gastroscope to facilitate balloon dilatation. Biopsies examined for immunofluorescence showed continuous linear deposition along the basement membrane zone for IgG and C3, consistent with atypical esophageal bullous systemic lupus erythematosus or atypical esophageal bullous pemphigoid. The patient declined systemic steroids. Her mycophenolate mofetil dose was increased and she received weekly dilatations to prevent Koebnerization and allow time for medical therapy effect. After three months of treatment, she had symptom improvement.
Discussion: In patients with systemic immune mediated disorders including rheumatological disease, bullous diseases can be considered as a cause of esophageal stricture. Bullous disease with esophageal involvement can be difficult to treat, especially in this patient who declined corticosteroids. A combination approach using both immune suppression and dilatation was effective.
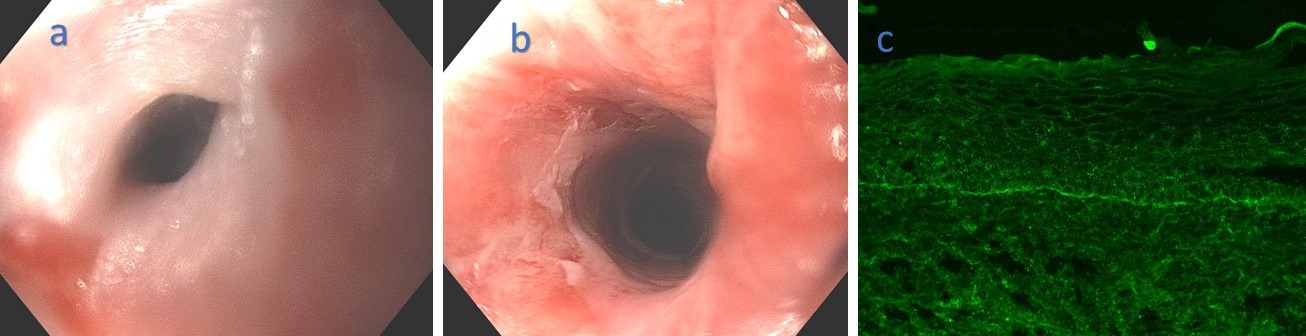
Figure: Figure1.
a. Pre- dilatation during repeated dilation treatments. Diameter 8mm.
b. Post- dilatation. Diameter 11mm.
c. Immunofluorescence showing IgG deposition along the basement membrane.
a. Pre- dilatation during repeated dilation treatments. Diameter 8mm.
b. Post- dilatation. Diameter 11mm.
c. Immunofluorescence showing IgG deposition along the basement membrane.
Disclosures:
Caroline Olson indicated no relevant financial relationships.
Haily Vora indicated no relevant financial relationships.
Paul Kröner indicated no relevant financial relationships.
Maoyin Pang indicated no relevant financial relationships.
Caroline Olson, MD, Haily Vora, MD, MPH, Paul Kröner, MD, MS, Maoyin Pang, MD, PhD. D0231 - Esophageal Stricture Recalcitrant to Repeated Dilation in Complex Rheumatological and Bullous Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

