Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0235 - Time for a Rendezvous: Multi-Disciplinary Management of Complete Esophageal Obstruction in a Patient Following Radiation to Post-Surgical Anatomy
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- SS
Shabari M. Shenoy, MBBS
Icahn School of Medicine at Mount Sinai Morningside-West
new york, NY
Presenting Author(s)
Shabari M. Shenoy, MBBS1, Gres Karim, MD2, Kimberly Cavaliere, MD3, Michael S. Smith, MD, MBA4
1Icahn School of Medicine at Mount Sinai Morningside-West, New York, NY; 2Mount Sinai Beth Israel, New York, NY; 3Mount Sinai, New York, NY; 4Mount Sinai Morningside and Mount Sinai West Hospitals, New York, NY
Introduction: Esophageal stricture is a common complication of radiation exposure. Balloon dilation restores luminal patency for partial narrowing, though complete obstruction can require recanalization through combined anterograde and retrograde endoscopic dilation (CARD), also known as the rendezvous technique. We describe a case of successful CARD recanalization following multimodal cancer treatment.
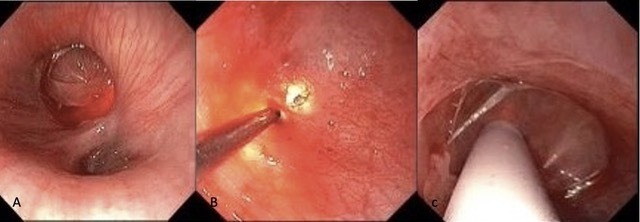
Case Description/Methods: A 65-year-old male with right tonsillar cancer underwent resection of the right tonsil, tongue base and palate with pectoralis major reconstruction, followed by radiation. One year later, he reported progressive dysphagia to solids and liquids that required gastrostomy tube placement to maintain adequate nutrition. Laryngoscopy revealed radiation changes but no evidence of malignancy, and upper endoscopy revealed complete luminal obstruction. Retrograde endoscopy via gastrostomy initially was unsuccessful due to scarring, so wire-guided Savary dilation was performed until an ultra-thin endoscope could pass into the stomach. Retrograde inspection revealed a benign-appearing, complete stenosis in the proximal esophagus. Concurrent antegrade laryngoscopy visualized a thin tissue membrane with distal endoscopic illumination. The membrane was pierced retrograde under direct visualization with the sharp end of a Savary wire, after which it was advanced out the mouth. Stepwise antegrade Savary dilation then was performed over this wire to 45 French under visualization with the retrograde endoscope. Post-dilation inspection showed moderate mucosal disruption without luminal perforation, significant improvement in luminal narrowing, and minimal bleeding. A 12 French nasogastric tube was placed to maintain luminal patency, and the patient was discharged home. While he regained the ability to swallow liquids, a second dilation session was required to achieve complete dysphagia relief.
Discussion: Most CARD procedures are performed by gastroenterologists to treat post-radiation luminal obstruction. However, this case demonstrates CARD can be performed collaboratively with surgeons, which can be helpful in the setting of post-operative anatomy. CARD is effective, safe, and well-tolerated, with a lower complication risk (esophageal perforation, pneumomediastinum) compared to blind antegrade dilation. High technical success rates (83%) and frequent dysphagia resolution (44%) make CARD a preferred approach to restore luminal patency in patients with severe radiation-induced dysphagia.
Disclosures:
Shabari M. Shenoy, MBBS1, Gres Karim, MD2, Kimberly Cavaliere, MD3, Michael S. Smith, MD, MBA4. D0235 - Time for a Rendezvous: Multi-Disciplinary Management of Complete Esophageal Obstruction in a Patient Following Radiation to Post-Surgical Anatomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai Morningside-West, New York, NY; 2Mount Sinai Beth Israel, New York, NY; 3Mount Sinai, New York, NY; 4Mount Sinai Morningside and Mount Sinai West Hospitals, New York, NY
Introduction: Esophageal stricture is a common complication of radiation exposure. Balloon dilation restores luminal patency for partial narrowing, though complete obstruction can require recanalization through combined anterograde and retrograde endoscopic dilation (CARD), also known as the rendezvous technique. We describe a case of successful CARD recanalization following multimodal cancer treatment.
Case Description/Methods: A 65-year-old male with right tonsillar cancer underwent resection of the right tonsil, tongue base and palate with pectoralis major reconstruction, followed by radiation. One year later, he reported progressive dysphagia to solids and liquids that required gastrostomy tube placement to maintain adequate nutrition. Laryngoscopy revealed radiation changes but no evidence of malignancy, and upper endoscopy revealed complete luminal obstruction. Retrograde endoscopy via gastrostomy initially was unsuccessful due to scarring, so wire-guided Savary dilation was performed until an ultra-thin endoscope could pass into the stomach. Retrograde inspection revealed a benign-appearing, complete stenosis in the proximal esophagus. Concurrent antegrade laryngoscopy visualized a thin tissue membrane with distal endoscopic illumination. The membrane was pierced retrograde under direct visualization with the sharp end of a Savary wire, after which it was advanced out the mouth. Stepwise antegrade Savary dilation then was performed over this wire to 45 French under visualization with the retrograde endoscope. Post-dilation inspection showed moderate mucosal disruption without luminal perforation, significant improvement in luminal narrowing, and minimal bleeding. A 12 French nasogastric tube was placed to maintain luminal patency, and the patient was discharged home. While he regained the ability to swallow liquids, a second dilation session was required to achieve complete dysphagia relief.
Discussion: Most CARD procedures are performed by gastroenterologists to treat post-radiation luminal obstruction. However, this case demonstrates CARD can be performed collaboratively with surgeons, which can be helpful in the setting of post-operative anatomy. CARD is effective, safe, and well-tolerated, with a lower complication risk (esophageal perforation, pneumomediastinum) compared to blind antegrade dilation. High technical success rates (83%) and frequent dysphagia resolution (44%) make CARD a preferred approach to restore luminal patency in patients with severe radiation-induced dysphagia.
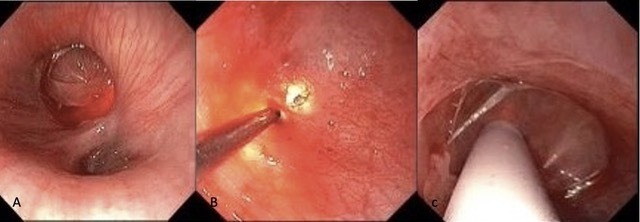
Figure: A- Stricture in the upper third of the esophagus; B- Piercing of the membrane in the upper third of the esophagus; C- Savary dilation of the upper third of the esophagus
Disclosures:
Shabari Shenoy indicated no relevant financial relationships.
Gres Karim indicated no relevant financial relationships.
Kimberly Cavaliere indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Advisory Committee/Board Member. CDx Diagnostics – Advisory Committee/Board Member, Consultant. GI Supply – Consultant. Lucid Diagnostics – Advisory Committee/Board Member, Consultant. Steris Endoscopy – Consultant.
Shabari M. Shenoy, MBBS1, Gres Karim, MD2, Kimberly Cavaliere, MD3, Michael S. Smith, MD, MBA4. D0235 - Time for a Rendezvous: Multi-Disciplinary Management of Complete Esophageal Obstruction in a Patient Following Radiation to Post-Surgical Anatomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
