Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0236 - The Marching Band: Pseudoachalasia Secondary to Gastric Band Slippage
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- SS
Shabari M. Shenoy, MBBS
Icahn School of Medicine at Mount Sinai Morningside-West
new york, NY
Presenting Author(s)
Shabari M. Shenoy, MBBS1, Gres Karim, MD2, Kimberly Cavaliere, MD3
1Icahn School of Medicine at Mount Sinai Morningside-West, New York, NY; 2Mount Sinai Beth Israel, New York, NY; 3Mount Sinai, New York, NY
Introduction: Gastric band slippage is a late complication of laparoscopic adjustable gastric banding surgery (LAGBS) with an incidence of less than 5%. We present a case of pseudoachalasia caused by gastric band slippage in a patient with a history of LAGBS.
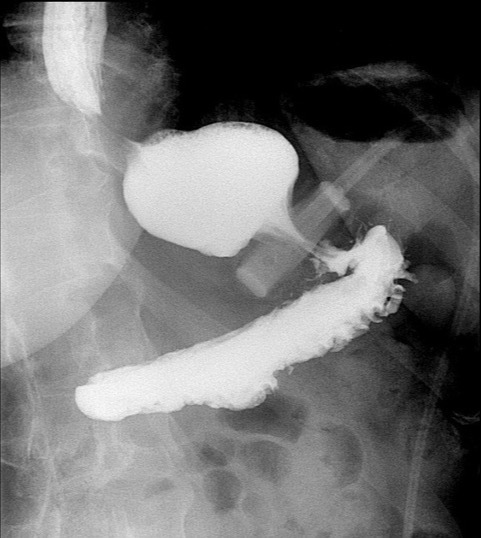
Case Description/Methods: A 53-year-old female with a history of LAGBS for obesity ten years ago presented to our motility clinic with complaints of recurrent emesis for the last ten years. Episodes were associated with minimal retching, often self-induced to relieve chest discomfort. She appeared tearful while explaining the debility from her symptoms, severely affecting her quality of life. Due to severe, progressive worsening of symptoms for three months prior to presentation, a gastric emptying study performed by her gastroenterologist did not reveal any pathology. A recent esophagogastroduodenoscopy showed mild esophagitis. Proton pump inhibitors provided no relief. Given the incongruence between symptoms and workup, we decided to obtain an upper gastrointestinal (UGI) series. UGI series revealed tilting of the laparoscopic band, collimation around the thoracic esophagus immediately on barium swallow followed by passage of short amount of contrast along the narrowed diameter at the location of the band. Over the course of the study, significant stasis was noted in the thoracic esophagus causing severe restriction of passage confirming the diagnosis of gastric band slippage. She was referred to bariatric surgery for adjustment of the gastric band.
Discussion: The complication rate from LAGBS increases by 3-4% each year that the band is left in-vivo and rises to 40% at 10 years. Complications such as slippage and obstruction at the band site present with nonspecific symptoms such as vomiting and regurgitation. In our patient’s case, pseudoachalasia was one of the differential diagnoses given the long-standing dysphagia, regurgitation, and chest discomfort. Although majority of pseudoachalasia is cancer related, benign causes also exist. LAGB can lead to formation of scar tissue from tight fundic band can also cause pseudoachalasia by creating persistent high-pressure and low flow resistance, leading to impaired LES relaxation, weakening of the esophageal body. This case highlights the importance of primary care providers and gastroenterologists familiarizing themselves with presentation, diagnosis, and management of late complications of bariatric procedures as delayed diagnosis can severely affect quality of life as demonstrated by our case.
Disclosures:
Shabari M. Shenoy, MBBS1, Gres Karim, MD2, Kimberly Cavaliere, MD3. D0236 - The Marching Band: Pseudoachalasia Secondary to Gastric Band Slippage, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai Morningside-West, New York, NY; 2Mount Sinai Beth Israel, New York, NY; 3Mount Sinai, New York, NY
Introduction: Gastric band slippage is a late complication of laparoscopic adjustable gastric banding surgery (LAGBS) with an incidence of less than 5%. We present a case of pseudoachalasia caused by gastric band slippage in a patient with a history of LAGBS.
Case Description/Methods: A 53-year-old female with a history of LAGBS for obesity ten years ago presented to our motility clinic with complaints of recurrent emesis for the last ten years. Episodes were associated with minimal retching, often self-induced to relieve chest discomfort. She appeared tearful while explaining the debility from her symptoms, severely affecting her quality of life. Due to severe, progressive worsening of symptoms for three months prior to presentation, a gastric emptying study performed by her gastroenterologist did not reveal any pathology. A recent esophagogastroduodenoscopy showed mild esophagitis. Proton pump inhibitors provided no relief. Given the incongruence between symptoms and workup, we decided to obtain an upper gastrointestinal (UGI) series. UGI series revealed tilting of the laparoscopic band, collimation around the thoracic esophagus immediately on barium swallow followed by passage of short amount of contrast along the narrowed diameter at the location of the band. Over the course of the study, significant stasis was noted in the thoracic esophagus causing severe restriction of passage confirming the diagnosis of gastric band slippage. She was referred to bariatric surgery for adjustment of the gastric band.
Discussion: The complication rate from LAGBS increases by 3-4% each year that the band is left in-vivo and rises to 40% at 10 years. Complications such as slippage and obstruction at the band site present with nonspecific symptoms such as vomiting and regurgitation. In our patient’s case, pseudoachalasia was one of the differential diagnoses given the long-standing dysphagia, regurgitation, and chest discomfort. Although majority of pseudoachalasia is cancer related, benign causes also exist. LAGB can lead to formation of scar tissue from tight fundic band can also cause pseudoachalasia by creating persistent high-pressure and low flow resistance, leading to impaired LES relaxation, weakening of the esophageal body. This case highlights the importance of primary care providers and gastroenterologists familiarizing themselves with presentation, diagnosis, and management of late complications of bariatric procedures as delayed diagnosis can severely affect quality of life as demonstrated by our case.
Figure: UGI series demonstrating tilting of the laparoscopic band, collimation around the thoracic esophagus immediately on barium swallow along the narrowed diameter at the location of the band.
Disclosures:
Shabari Shenoy indicated no relevant financial relationships.
Gres Karim indicated no relevant financial relationships.
Kimberly Cavaliere indicated no relevant financial relationships.
Shabari M. Shenoy, MBBS1, Gres Karim, MD2, Kimberly Cavaliere, MD3. D0236 - The Marching Band: Pseudoachalasia Secondary to Gastric Band Slippage, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
