Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0030 - A Case of Secondary Sclerosing Cholangitis Due to Polytrauma
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Sylvia Keiser, DO
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Sylvia Keiser, DO, Landon Brown, MD, Pranav Penninti, DO, Laura Rosenkranz, MD
University of Texas Health San Antonio, San Antonio, TX
Introduction: Secondary sclerosing cholangitis (SSC) is a cholestatic biliary disease characterized by inflammation, fibrosis, stricture formation and ultimately destruction of the biliary tree leading to cirrhosis. SSC can appear morphologically similar to other biliary pathologies such as primary sclerosing cholangitis (PSC). However, unlike PSC, SSC is secondary to an underlying identifiable pathological process. We present a case of SSC occurring in the setting of a critically ill patient with polytrauma.
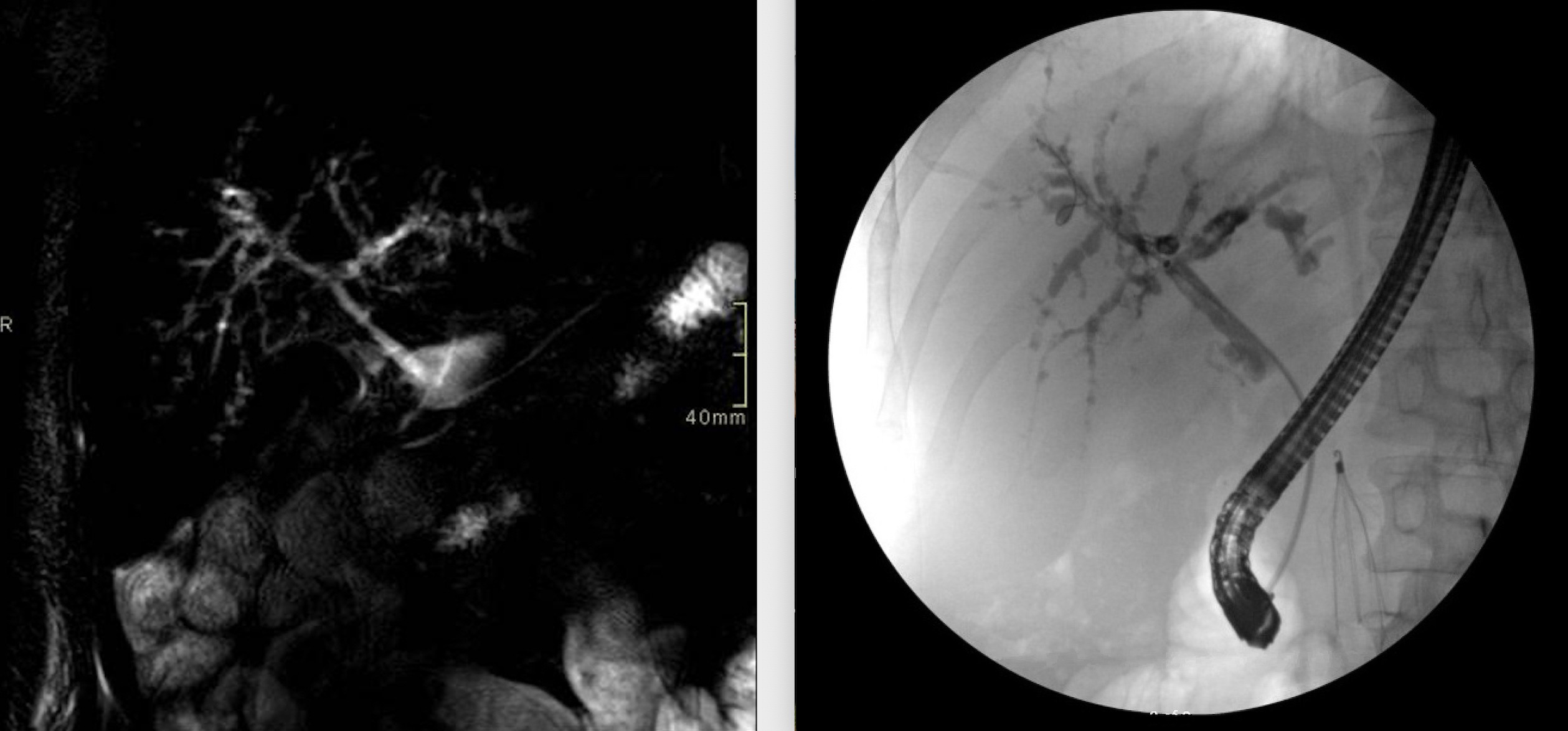
Case Description/Methods: A 48-year-old male with no past medical history presented to the emergency room after a motorcycle accident. The patient sustained many injuries including several orthopedic fractures and vascular injuries. He was admitted to the intensive care unit and underwent multiple surgeries. The patient’s hospital course was complicated by several infections and septic shock. He also required ECMO and CRRT due to subsequent renal and cardiovascular failure. During his hospitalization, he developed persistent elevation of his liver enzymes, most notably his alkaline phosphatase (greater than 2,000U/L). An MRCP was performed and demonstrated intrahepatic biliary dilation with suspected multifocal areas of beading, which were not present on his initial abdominal imaging. A subsequent liver biopsy was obtained and showed prominent ductal proliferation with cholestasis. Gastroenterology was consulted and the patient underwent an ERCP which showed dilated intrahepatic ducts along with a beaded appearance. He was found to have an elevated IgG4 at 260mg/dL, raising the possibly of IgG4-mediated cholangiopathy. The patient’s alkaline phosphatase began to downtrend and he was discharged home with close hepatology follow up.
Discussion: The most common causes of SSC include surgical or blunt biliary trauma, ischemic injury, intra-arterial chemotherapy, and recurrent pancreatitis. In order to diagnose a patient with PSC, one must first exclude secondary causes. Our patient’s imaging demonstrated findings consistent with PSC; however, prior to his accident these findings were absent. He was found to have an elevated IgG4; however, the pathology from his liver biopsy did not demonstrate lymphoplasmacytic infiltration. Given the patient’s history of polytrauma, septic shock, and overall critical illness, we suspect that he developed SSC. It is imperative for gastroenterologists to consider SSC on the differential of cholestasis as early diagnosis and treatment is associated with improved prognosis.
Disclosures:
Sylvia Keiser, DO, Landon Brown, MD, Pranav Penninti, DO, Laura Rosenkranz, MD. B0030 - A Case of Secondary Sclerosing Cholangitis Due to Polytrauma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Texas Health San Antonio, San Antonio, TX
Introduction: Secondary sclerosing cholangitis (SSC) is a cholestatic biliary disease characterized by inflammation, fibrosis, stricture formation and ultimately destruction of the biliary tree leading to cirrhosis. SSC can appear morphologically similar to other biliary pathologies such as primary sclerosing cholangitis (PSC). However, unlike PSC, SSC is secondary to an underlying identifiable pathological process. We present a case of SSC occurring in the setting of a critically ill patient with polytrauma.
Case Description/Methods: A 48-year-old male with no past medical history presented to the emergency room after a motorcycle accident. The patient sustained many injuries including several orthopedic fractures and vascular injuries. He was admitted to the intensive care unit and underwent multiple surgeries. The patient’s hospital course was complicated by several infections and septic shock. He also required ECMO and CRRT due to subsequent renal and cardiovascular failure. During his hospitalization, he developed persistent elevation of his liver enzymes, most notably his alkaline phosphatase (greater than 2,000U/L). An MRCP was performed and demonstrated intrahepatic biliary dilation with suspected multifocal areas of beading, which were not present on his initial abdominal imaging. A subsequent liver biopsy was obtained and showed prominent ductal proliferation with cholestasis. Gastroenterology was consulted and the patient underwent an ERCP which showed dilated intrahepatic ducts along with a beaded appearance. He was found to have an elevated IgG4 at 260mg/dL, raising the possibly of IgG4-mediated cholangiopathy. The patient’s alkaline phosphatase began to downtrend and he was discharged home with close hepatology follow up.
Discussion: The most common causes of SSC include surgical or blunt biliary trauma, ischemic injury, intra-arterial chemotherapy, and recurrent pancreatitis. In order to diagnose a patient with PSC, one must first exclude secondary causes. Our patient’s imaging demonstrated findings consistent with PSC; however, prior to his accident these findings were absent. He was found to have an elevated IgG4; however, the pathology from his liver biopsy did not demonstrate lymphoplasmacytic infiltration. Given the patient’s history of polytrauma, septic shock, and overall critical illness, we suspect that he developed SSC. It is imperative for gastroenterologists to consider SSC on the differential of cholestasis as early diagnosis and treatment is associated with improved prognosis.
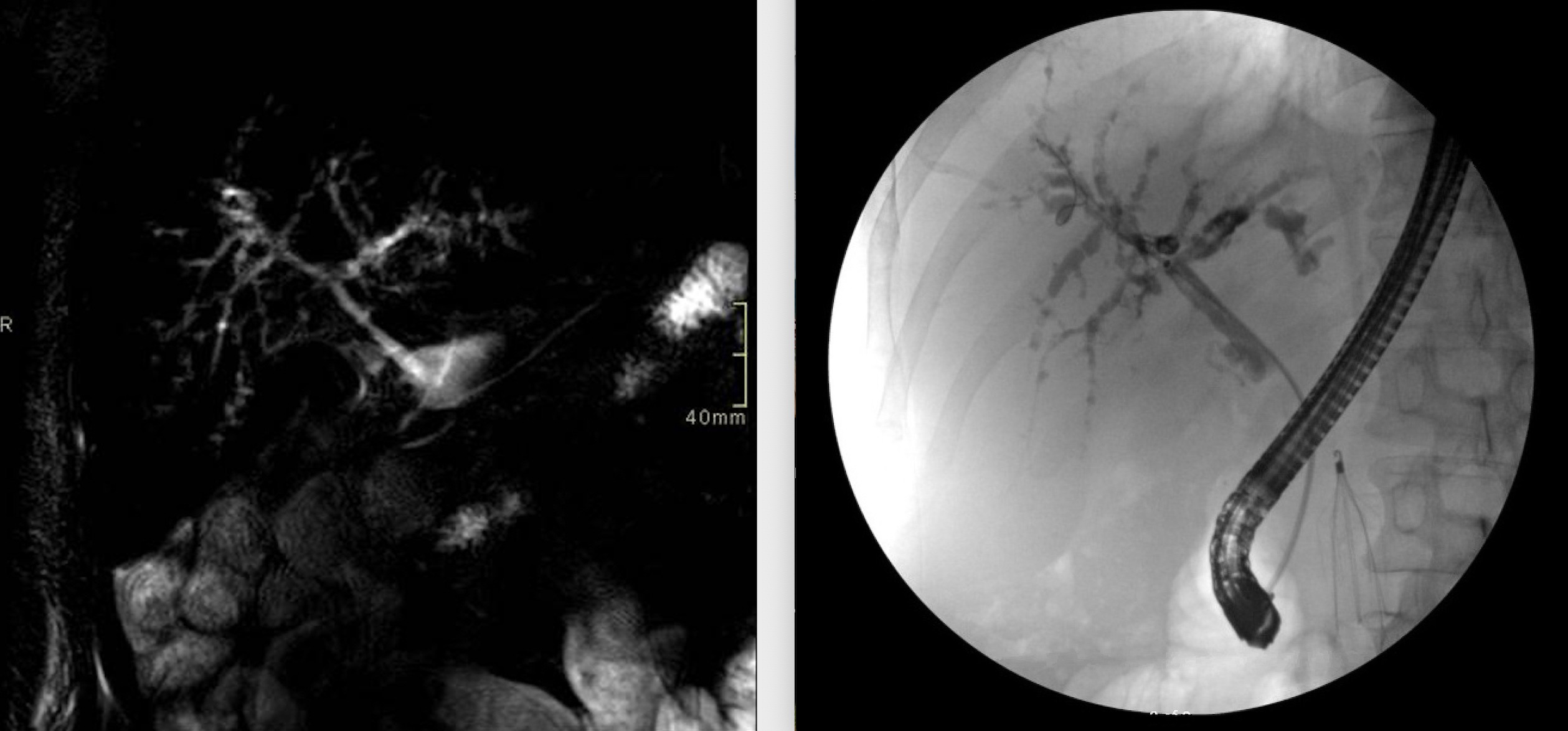
Figure: MRCP and ERCP showing dilated intrahepatic ducts with multifocal areas of beading.
Disclosures:
Sylvia Keiser indicated no relevant financial relationships.
Landon Brown indicated no relevant financial relationships.
Pranav Penninti indicated no relevant financial relationships.
Laura Rosenkranz indicated no relevant financial relationships.
Sylvia Keiser, DO, Landon Brown, MD, Pranav Penninti, DO, Laura Rosenkranz, MD. B0030 - A Case of Secondary Sclerosing Cholangitis Due to Polytrauma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
