Back

Poster Session A - Sunday Afternoon
Category: IBD
A0411 - Not Just Another Infection: Rare Case Abscess in Ulcerative Colitis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Jonathan E. Selzman, DO
University of Texas Health Science Center
San Antonio, TX
Presenting Author(s)
Jonathan E. Selzman, DO1, Sanjay Prasad, MD2, Mahesh Gajendran, MD, MPH3, Nagasri Shankar, MD4, Brenda M. Briones, MD2, Patrick Snyder, MD4, Dhruv Mehta, MD1, Chandraprakash Umapathy, MD5, Juan Echavarria, MS, MD5
1University of Texas Health Science Center , San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX; 3UTHSCSA, San Antonio, TX; 4UT Health San Antonio, San Antonio, TX; 5University of Texas Health San Antonio, San Antonio, TX
Introduction: Aseptic abscess syndrome (AAS) is a rare manifestation of inflammatory bowel disease (IBD). This condition is characterized by sterile neutrophilic infiltration of deep tissues, most often in the spleen, liver, skin, or lymph nodes. Patients commonly present with fever, abdominal pain, and weight loss. We present a case of a 40-year-old female diagnosed with AAS in the setting of IBD.
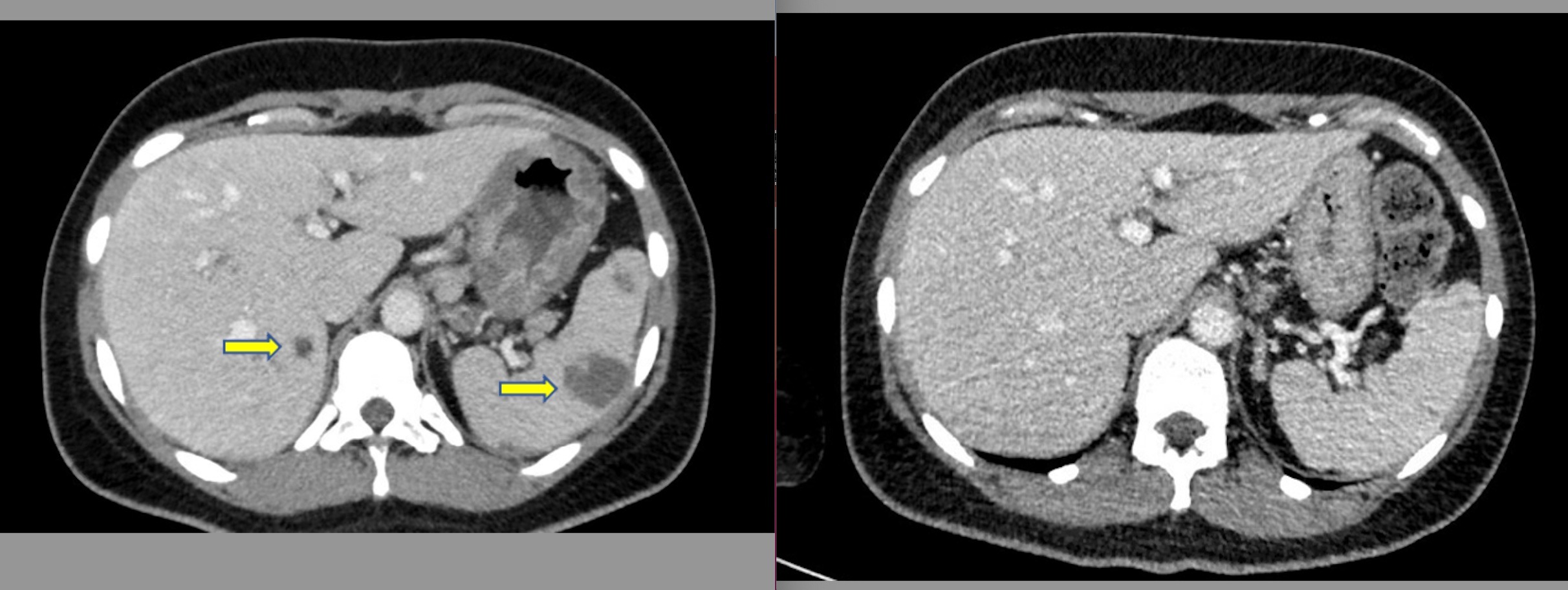
Case Description/Methods: A 40-year-old female with a history of Ulcerative Colitis (UC) not on treatment for past 2 years presented with 2 weeks of bloody diarrhea, left-sided abdominal pain, unintentional weight loss, and fatigue. On exam, she was tachycardic, normotensive, and had left lower quadrant abdominal tenderness. Initial lab work was significant for leukocytosis of 23.3 × 109 /L and elevated C-reactive protein. Computed tomography (CT) scan of the abdomen demonstrated diffuse colonic thickening and multiple hepatosplenic abscesses. Broad-spectrum antibiotics were initiated. She underwent colonoscopy which revealed Mayo 2 colitis from rectum to the distal transverse colon. Blood cultures (fungal, bacterial, and mycobacterial) and parasitic serologies were negative. Fluid aspiration from the spleen drained purulent material, but fluid cultures were negative. Despite treatment with broad-spectrum antibiotics, and antifungals, the patient continued to remain febrile with persistent leukocytosis and gastrointestinal symptoms. After ruling out infectious and neoplastic processes, a diagnosis of aseptic abscess syndrome was made. Systemic steroids were initiated with resulting improvement in her symptoms and lab parameters. The patient was discharged home on a steroid taper. Repeat cross-sectional imaging performed 3 weeks post-discharge demonstrated complete resolution of all abscesses. For UC, she was started on Vedolizumab and she remains in clinical remission.
Discussion: AAS is a diagnosis of exclusion. This syndrome should be considered in IBD patients in the setting of multiple disseminated abscesses with a negative infectious work-up and lack of clinical improvement with antimicrobial agents. The specific pathophysiology is largely unknown, although similar neutrophilic infiltration can be seen in pyoderma gangrenosum. Antibiotic therapy is universally ineffective for AAS. However, about 95 % of patients respond to corticosteroids. Disease-modifying agents and biologics have been successfully used as maintenance therapy.
Disclosures:
Jonathan E. Selzman, DO1, Sanjay Prasad, MD2, Mahesh Gajendran, MD, MPH3, Nagasri Shankar, MD4, Brenda M. Briones, MD2, Patrick Snyder, MD4, Dhruv Mehta, MD1, Chandraprakash Umapathy, MD5, Juan Echavarria, MS, MD5. A0411 - Not Just Another Infection: Rare Case Abscess in Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Texas Health Science Center , San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX; 3UTHSCSA, San Antonio, TX; 4UT Health San Antonio, San Antonio, TX; 5University of Texas Health San Antonio, San Antonio, TX
Introduction: Aseptic abscess syndrome (AAS) is a rare manifestation of inflammatory bowel disease (IBD). This condition is characterized by sterile neutrophilic infiltration of deep tissues, most often in the spleen, liver, skin, or lymph nodes. Patients commonly present with fever, abdominal pain, and weight loss. We present a case of a 40-year-old female diagnosed with AAS in the setting of IBD.
Case Description/Methods: A 40-year-old female with a history of Ulcerative Colitis (UC) not on treatment for past 2 years presented with 2 weeks of bloody diarrhea, left-sided abdominal pain, unintentional weight loss, and fatigue. On exam, she was tachycardic, normotensive, and had left lower quadrant abdominal tenderness. Initial lab work was significant for leukocytosis of 23.3 × 109 /L and elevated C-reactive protein. Computed tomography (CT) scan of the abdomen demonstrated diffuse colonic thickening and multiple hepatosplenic abscesses. Broad-spectrum antibiotics were initiated. She underwent colonoscopy which revealed Mayo 2 colitis from rectum to the distal transverse colon. Blood cultures (fungal, bacterial, and mycobacterial) and parasitic serologies were negative. Fluid aspiration from the spleen drained purulent material, but fluid cultures were negative. Despite treatment with broad-spectrum antibiotics, and antifungals, the patient continued to remain febrile with persistent leukocytosis and gastrointestinal symptoms. After ruling out infectious and neoplastic processes, a diagnosis of aseptic abscess syndrome was made. Systemic steroids were initiated with resulting improvement in her symptoms and lab parameters. The patient was discharged home on a steroid taper. Repeat cross-sectional imaging performed 3 weeks post-discharge demonstrated complete resolution of all abscesses. For UC, she was started on Vedolizumab and she remains in clinical remission.
Discussion: AAS is a diagnosis of exclusion. This syndrome should be considered in IBD patients in the setting of multiple disseminated abscesses with a negative infectious work-up and lack of clinical improvement with antimicrobial agents. The specific pathophysiology is largely unknown, although similar neutrophilic infiltration can be seen in pyoderma gangrenosum. Antibiotic therapy is universally ineffective for AAS. However, about 95 % of patients respond to corticosteroids. Disease-modifying agents and biologics have been successfully used as maintenance therapy.
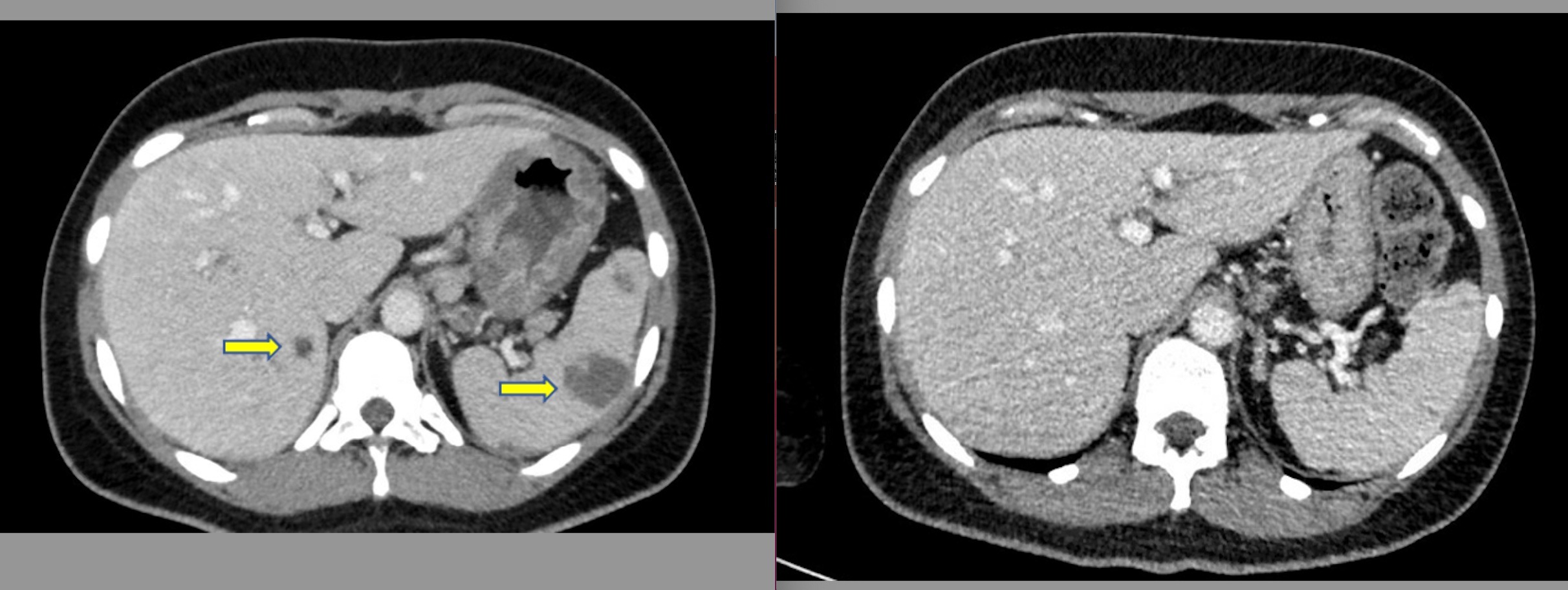
Figure: Initial and subsequent CT imaging of abdomen/pelvis with contrast demonstrating hepatic and splenic abscesses with interval improvement of abscess
Disclosures:
Jonathan Selzman indicated no relevant financial relationships.
Sanjay Prasad indicated no relevant financial relationships.
Mahesh Gajendran indicated no relevant financial relationships.
Nagasri Shankar indicated no relevant financial relationships.
Brenda Briones indicated no relevant financial relationships.
Patrick Snyder indicated no relevant financial relationships.
Dhruv Mehta indicated no relevant financial relationships.
Chandraprakash Umapathy indicated no relevant financial relationships.
Juan Echavarria indicated no relevant financial relationships.
Jonathan E. Selzman, DO1, Sanjay Prasad, MD2, Mahesh Gajendran, MD, MPH3, Nagasri Shankar, MD4, Brenda M. Briones, MD2, Patrick Snyder, MD4, Dhruv Mehta, MD1, Chandraprakash Umapathy, MD5, Juan Echavarria, MS, MD5. A0411 - Not Just Another Infection: Rare Case Abscess in Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
