Back

Poster Session A - Sunday Afternoon
Category: GI Bleeding
A0317 - Primary Aortoenteric Fistula: A Rare Presentation of a Herald Bleed
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Davis B. Berry, DO
East Tennessee State University
Johnson City, Tennessee
Presenting Author(s)
Davis B. Berry, DO, Andrew Canning, MD, Mark Young, MD
East Tennessee State University, Johnson City, TN
Introduction: Rarely, an aortoenteric fistula (AEF) is identified as the source of a herald bleed, or one that precedes a catastrophic hemorrhagic event such as abdominal aortic aneurysm rupture. AEFs are abnormal communications between the GI tract and aorta that arise most commonly secondary to aortic vascular procedures. In contrast, primary AEFs have much lower incidence and are felt to arise spontaneously from erosion.
Case Description/Methods: We present a 69 year old female with prior history of an abdominal aortic aneurysm who presented with multiple bouts of hematemesis and abdominal pain. CT showed an irregular shaped infrarenal abdominal aortic aneurysm with dimensions 9.6 x 7.5 cm with evidence of contained rupture. The patient developed hemorrhagic shock with both hematemesis and brisk hematochezia.
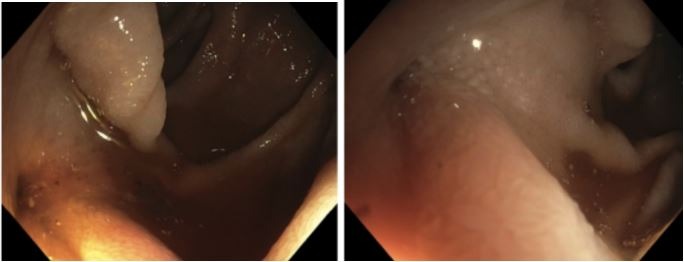
With stabilization, the patient underwent percutaneous endovascular aneurysm repair with stent placement over aortic bifurcation. Following vascular intervention, no further hematemesis or clinical GI bleeding occurred. Push enteroscopy was performed revealing a defect in the distal third portion of the duodenum with extravasation of both debris and blood (image 1). The ampulla was excluded as a bleeding source. This mucosal defect was concerning for AEF and hemoclips were deployed to mark its location. Following this hospitalization, the patient later died from chronic respiratory failure.
Discussion: This case presents a “herald” GI bleed secondary to a primary aortoenteric fistula. A classic triad of abdominal pain, pulsating mass and gastrointestinal bleeding has been described, however all 3 components are present in a minority of cases. Primary AEFs have a commonly cited incidence of 0.07%. Identification of both primary and secondary AEF demands a high index of suspicion, particularly in the setting of acute aneurysm.
Endoscopically confirming aortoenteric fistula is technically challenging and often inconclusive, thus CT with contrast is preferred with sensitivity 94% and specificity 85%. Presence of air bubbles or intravascular air on CT is often confirmatory. With an estimated mortality rate of primary AEF of approximately 36%, surgical management is usually required. Surgical options include utilizing an in situ graft versus direct closure of the mucosal defect in the GI tract. Endovascular techniques including aortic stent and graft placement are increasingly used.
Disclosures:
Davis B. Berry, DO, Andrew Canning, MD, Mark Young, MD. A0317 - Primary Aortoenteric Fistula: A Rare Presentation of a Herald Bleed, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
East Tennessee State University, Johnson City, TN
Introduction: Rarely, an aortoenteric fistula (AEF) is identified as the source of a herald bleed, or one that precedes a catastrophic hemorrhagic event such as abdominal aortic aneurysm rupture. AEFs are abnormal communications between the GI tract and aorta that arise most commonly secondary to aortic vascular procedures. In contrast, primary AEFs have much lower incidence and are felt to arise spontaneously from erosion.
Case Description/Methods: We present a 69 year old female with prior history of an abdominal aortic aneurysm who presented with multiple bouts of hematemesis and abdominal pain. CT showed an irregular shaped infrarenal abdominal aortic aneurysm with dimensions 9.6 x 7.5 cm with evidence of contained rupture. The patient developed hemorrhagic shock with both hematemesis and brisk hematochezia.
With stabilization, the patient underwent percutaneous endovascular aneurysm repair with stent placement over aortic bifurcation. Following vascular intervention, no further hematemesis or clinical GI bleeding occurred. Push enteroscopy was performed revealing a defect in the distal third portion of the duodenum with extravasation of both debris and blood (image 1). The ampulla was excluded as a bleeding source. This mucosal defect was concerning for AEF and hemoclips were deployed to mark its location. Following this hospitalization, the patient later died from chronic respiratory failure.
Discussion: This case presents a “herald” GI bleed secondary to a primary aortoenteric fistula. A classic triad of abdominal pain, pulsating mass and gastrointestinal bleeding has been described, however all 3 components are present in a minority of cases. Primary AEFs have a commonly cited incidence of 0.07%. Identification of both primary and secondary AEF demands a high index of suspicion, particularly in the setting of acute aneurysm.
Endoscopically confirming aortoenteric fistula is technically challenging and often inconclusive, thus CT with contrast is preferred with sensitivity 94% and specificity 85%. Presence of air bubbles or intravascular air on CT is often confirmatory. With an estimated mortality rate of primary AEF of approximately 36%, surgical management is usually required. Surgical options include utilizing an in situ graft versus direct closure of the mucosal defect in the GI tract. Endovascular techniques including aortic stent and graft placement are increasingly used.
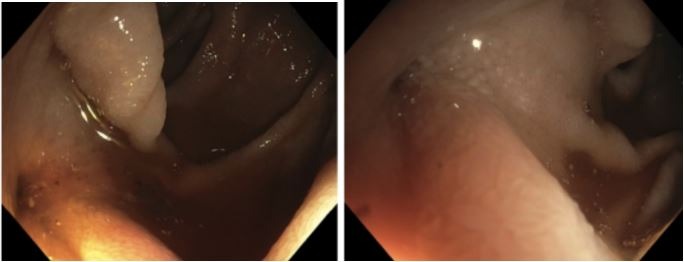
Figure: Defect in duodenal mucosa representing primary aortoenteric fistula
Disclosures:
Davis Berry indicated no relevant financial relationships.
Andrew Canning indicated no relevant financial relationships.
Mark Young indicated no relevant financial relationships.
Davis B. Berry, DO, Andrew Canning, MD, Mark Young, MD. A0317 - Primary Aortoenteric Fistula: A Rare Presentation of a Herald Bleed, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
