Back

Poster Session B - Monday Morning
Category: Small Intestine
B0672 - A Rare Case of Autoimmune Enteropathy Misdiagnosed as Celiac Disease
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Munraj Singh, MD
Louisiana State University Health Sciences Center
New Orleans, LA
Presenting Author(s)
Munraj Singh, MD, Catherine Hudson, MD, MPH
Louisiana State University Health Sciences Center, New Orleans, LA
Introduction: Autoimmune enteropathy (AIE) is an increasingly rare condition characterized by immune mediated intestinal mucosal injury that manifests as intractable diarrhea. Originally thought to be a pediatric condition, increasing cases have been reported in the adult population. While AIE can affect all parts of the GI tract, the duodenum is the most common site of GI tract involvement. The management of AIE is centered around optimizing nutritional status in addition to steroids, immunosuppression and biologic agents.
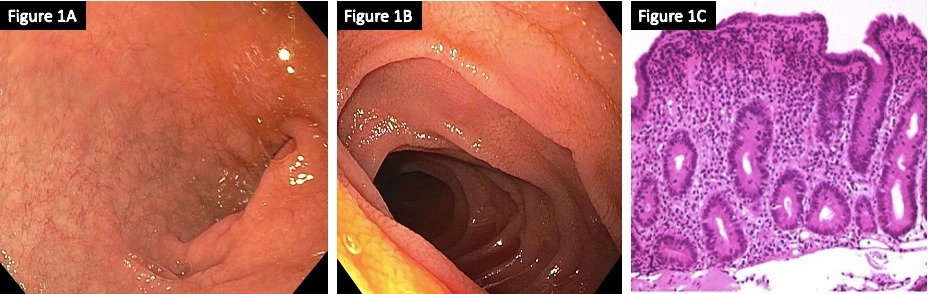
Case Description/Methods: A 29-year-old man with a childhood diagnosis of celiac disease presented for weakness and electrolyte abnormalities in the setting of chronic watery diarrhea. Laboratory findings were significant for WBC 6k uL, Potassium 2.5 mmol/L, Chloride 117 mmol/L, Creatinine 2.43 mg/dL, and decreased levels of Vitamins A, B, E, Zinc. Further investigation showed negative Tissue Transglutaminase IgA and negative workup for C. diff, Giardia, Cryptosporidium, and Campylobacter. Endoscopic evaluation showed atrophic duodenitis with erythema but no endoscopic evidence of celiac disease (Figure 1A,B). Histological examination of duodenal biopsies showed loss of goblet cells and Paneth cells in addition to villous blunting, intraepithelial lymphocytosis and increased apoptotic bodies consistent with AIE (Figure 1C).
Discussion: Among the causes of chronic diarrhea and malabsorption, AIE is a rare disorder that is often misdiagnosed and mistaken for celiac disease or IBD. The pathophysiology of AIE is related to abnormal expression of self-antigens on mucosal epithelial cells, activating CD4 T lymphocytes, which leads to the destruction of enterocytes through cytotoxic effects and apoptosis. Immunohistological studies have shown that autoantibodies can be directed against enterocytes and goblet cells but are not pathognomonic for AIE. Endoscopic findings include mucosal hyperemia, ulcerations and mucosal atrophy. While difficult, the management of AIE is centered around managing malnutrition and treating the underlying autoimmune disorder. Initial recommended treatment includes corticosteroids, however, in refractory cases immunosuppressive therapy such as azathioprine, 6-mercaptopurine, and monoclonal antibodies have been shown to be beneficial. Highlighted by the case we present, AIE can be undiagnosed for years and establishing an early diagnosis is critical in reducing morbidity and improving long-term outcomes.
Disclosures:
Munraj Singh, MD, Catherine Hudson, MD, MPH. B0672 - A Rare Case of Autoimmune Enteropathy Misdiagnosed as Celiac Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Louisiana State University Health Sciences Center, New Orleans, LA
Introduction: Autoimmune enteropathy (AIE) is an increasingly rare condition characterized by immune mediated intestinal mucosal injury that manifests as intractable diarrhea. Originally thought to be a pediatric condition, increasing cases have been reported in the adult population. While AIE can affect all parts of the GI tract, the duodenum is the most common site of GI tract involvement. The management of AIE is centered around optimizing nutritional status in addition to steroids, immunosuppression and biologic agents.
Case Description/Methods: A 29-year-old man with a childhood diagnosis of celiac disease presented for weakness and electrolyte abnormalities in the setting of chronic watery diarrhea. Laboratory findings were significant for WBC 6k uL, Potassium 2.5 mmol/L, Chloride 117 mmol/L, Creatinine 2.43 mg/dL, and decreased levels of Vitamins A, B, E, Zinc. Further investigation showed negative Tissue Transglutaminase IgA and negative workup for C. diff, Giardia, Cryptosporidium, and Campylobacter. Endoscopic evaluation showed atrophic duodenitis with erythema but no endoscopic evidence of celiac disease (Figure 1A,B). Histological examination of duodenal biopsies showed loss of goblet cells and Paneth cells in addition to villous blunting, intraepithelial lymphocytosis and increased apoptotic bodies consistent with AIE (Figure 1C).
Discussion: Among the causes of chronic diarrhea and malabsorption, AIE is a rare disorder that is often misdiagnosed and mistaken for celiac disease or IBD. The pathophysiology of AIE is related to abnormal expression of self-antigens on mucosal epithelial cells, activating CD4 T lymphocytes, which leads to the destruction of enterocytes through cytotoxic effects and apoptosis. Immunohistological studies have shown that autoantibodies can be directed against enterocytes and goblet cells but are not pathognomonic for AIE. Endoscopic findings include mucosal hyperemia, ulcerations and mucosal atrophy. While difficult, the management of AIE is centered around managing malnutrition and treating the underlying autoimmune disorder. Initial recommended treatment includes corticosteroids, however, in refractory cases immunosuppressive therapy such as azathioprine, 6-mercaptopurine, and monoclonal antibodies have been shown to be beneficial. Highlighted by the case we present, AIE can be undiagnosed for years and establishing an early diagnosis is critical in reducing morbidity and improving long-term outcomes.
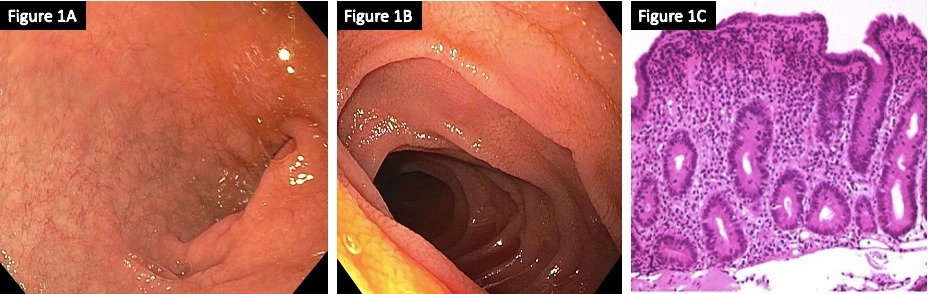
Figure: 1A: Duodenal bulb inflammation
1B: Erythema of 2nd portion of duodenum
1C: High power view of duodenal biopsy shows absent villi, expansion of the lamina propria with a lymphoplasmacytic infiltrate, and absence of goblet cells. Scattered intraepithelial lymphocytes and crypt apoptotic figures can be seen.
1B: Erythema of 2nd portion of duodenum
1C: High power view of duodenal biopsy shows absent villi, expansion of the lamina propria with a lymphoplasmacytic infiltrate, and absence of goblet cells. Scattered intraepithelial lymphocytes and crypt apoptotic figures can be seen.
Disclosures:
Munraj Singh indicated no relevant financial relationships.
Catherine Hudson indicated no relevant financial relationships.
Munraj Singh, MD, Catherine Hudson, MD, MPH. B0672 - A Rare Case of Autoimmune Enteropathy Misdiagnosed as Celiac Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
