Back

Poster Session D - Tuesday Morning
Category: GI Bleeding
D0333 - Gastrointestinal Hemorrhage With Gastritis and Pancolitis as Sole Presentation for Granulomatosis With Polyangiitis Flare
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Sarah Khan, MD
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Sarah Khan, MD1, Motasem Alkhayyat, MD2, Almaza A. Albakri, MD3, Sebouh Setrakian, MD2, Katherine Falloon, MD1, Mohannad Abou Saleh, MD2, Patricia Ajayi-Fox, MD2
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Royal Jordanian Medical Services, Amman, Al Karak, Jordan
Introduction: Granulomatosis with polyangiitis (GPA) is a rare small to medium vessel vasculitis. Estimated prevalence within the United Stated for GPA is 3/100,000 patients. The disease classically affects the upper respiratory tract, lungs and kidneys. Rarely, the gastrointestinal system is affected. In such cases, it is important to distinguish GPA from mimics, and diagnosis is guided by clinical judgement taken together with histologic analysis.
Case Description/Methods: A 27- year old male with history of GPA who presented with 2 weeks of bloody and black bowel movements associated with abdominal pain and bloody vomiting. Past history was notable for GPA diagnosed in childhood with presence of nasal inflammation, pulmonary nodules and rapidly progressive crescentic glomerulonephritis.
Initial laboratory analysis demonstrated leukocytosis to 13.6k/uL, elevated CRP to 2.5mg/and elevated Cr to 1.47mg/dL (baseline 1.07mg/dL). Abdominal CT scan revealed mesenteric lymphadenopathy, thickening and edema of the gastric antrum, suggestive of gastritis. Stool testing was positive for fecal calprotectin and lactoferrin, and negative for common bacterial pathogens. Serum C3 and C4 were normal, while testing for ANCA antibodies was negative, both on acute presentation and during routine testing previously.
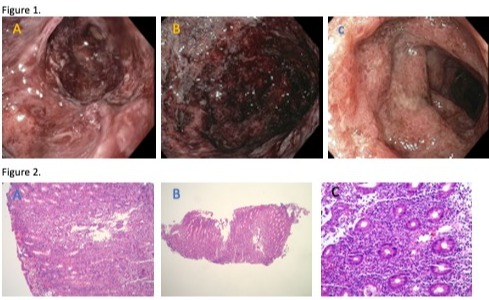
Endoscopy revealed striking hemorrhagic inflammation of the stomach, and colonoscopy showed pancolitis throughout examined colon. Gastric and colonic biopsies showed acute mucosal inflammation and non-necrotizing vasculitis, without granulomas. He was started on intravenous methylprednisolone, with rapid resolution of his symptoms thereafter. He was discharged on a prednisone taper and later transitioned to azathioprine therapy.
Discussion: Gastrointestinal manifestations of GPA are rare, with estimated prevalence of 6-7% of GPA patients. Gastrointestinal vasculitis causes inflammation with resulting end organ ischemia, leasing to a wide spectrum of clinical presentation. Predominantly intestinal manifestations are described, including mesenteric ischemia and bleeding. Thus, GI manifestations are associated with higher vasculitis severity on scoring indices, higher need for surgery and increased mortality. Interestingly, absence of granulomas on biopsy of the GI tract does not appear to be atypical. An important differential for gastrointestinal GPA is Crohn’s disease. Due to the paucity of data, current guidelines do not provide recommendations on management of GI manifestations on ANCA-associated vasculitis.
Disclosures:
Sarah Khan, MD1, Motasem Alkhayyat, MD2, Almaza A. Albakri, MD3, Sebouh Setrakian, MD2, Katherine Falloon, MD1, Mohannad Abou Saleh, MD2, Patricia Ajayi-Fox, MD2. D0333 - Gastrointestinal Hemorrhage With Gastritis and Pancolitis as Sole Presentation for Granulomatosis With Polyangiitis Flare, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Royal Jordanian Medical Services, Amman, Al Karak, Jordan
Introduction: Granulomatosis with polyangiitis (GPA) is a rare small to medium vessel vasculitis. Estimated prevalence within the United Stated for GPA is 3/100,000 patients. The disease classically affects the upper respiratory tract, lungs and kidneys. Rarely, the gastrointestinal system is affected. In such cases, it is important to distinguish GPA from mimics, and diagnosis is guided by clinical judgement taken together with histologic analysis.
Case Description/Methods: A 27- year old male with history of GPA who presented with 2 weeks of bloody and black bowel movements associated with abdominal pain and bloody vomiting. Past history was notable for GPA diagnosed in childhood with presence of nasal inflammation, pulmonary nodules and rapidly progressive crescentic glomerulonephritis.
Initial laboratory analysis demonstrated leukocytosis to 13.6k/uL, elevated CRP to 2.5mg/and elevated Cr to 1.47mg/dL (baseline 1.07mg/dL). Abdominal CT scan revealed mesenteric lymphadenopathy, thickening and edema of the gastric antrum, suggestive of gastritis. Stool testing was positive for fecal calprotectin and lactoferrin, and negative for common bacterial pathogens. Serum C3 and C4 were normal, while testing for ANCA antibodies was negative, both on acute presentation and during routine testing previously.
Endoscopy revealed striking hemorrhagic inflammation of the stomach, and colonoscopy showed pancolitis throughout examined colon. Gastric and colonic biopsies showed acute mucosal inflammation and non-necrotizing vasculitis, without granulomas. He was started on intravenous methylprednisolone, with rapid resolution of his symptoms thereafter. He was discharged on a prednisone taper and later transitioned to azathioprine therapy.
Discussion: Gastrointestinal manifestations of GPA are rare, with estimated prevalence of 6-7% of GPA patients. Gastrointestinal vasculitis causes inflammation with resulting end organ ischemia, leasing to a wide spectrum of clinical presentation. Predominantly intestinal manifestations are described, including mesenteric ischemia and bleeding. Thus, GI manifestations are associated with higher vasculitis severity on scoring indices, higher need for surgery and increased mortality. Interestingly, absence of granulomas on biopsy of the GI tract does not appear to be atypical. An important differential for gastrointestinal GPA is Crohn’s disease. Due to the paucity of data, current guidelines do not provide recommendations on management of GI manifestations on ANCA-associated vasculitis.
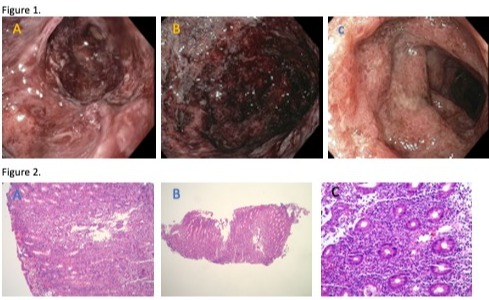
Figure: Figure 1. Endoscopic findings on endoscopy and colonoscopy. A, B. Hemorrhagic gastritis found on endoscopy. Diffuse severe hemorrhage with adherent blood and clots was found on the entire examined stomach. C. Colitis found on colonoscopy. The entire examined colon was characterized by diffuse severe inflammation with adherent blood, edema, erosions, erythema and granularity. Figure 2. A, B. Gastric mucosa. C. Colonic mucosa. The gastric oxyntic-type and colonic mucosa revealed an unusual pattern of chronic active gastritis and colitis with neutrophilic mediated epithelial injury in the form of glandular micro abscesses, cryptitis, crypt abscesses and vasculitis. No granulomas are identified. A Helicobacter pylori immunostaining was performed on the gastric biopsy, and it was negative.
Disclosures:
Sarah Khan indicated no relevant financial relationships.
Motasem Alkhayyat indicated no relevant financial relationships.
Almaza Albakri indicated no relevant financial relationships.
Sebouh Setrakian indicated no relevant financial relationships.
Katherine Falloon: Crohn's and Colitis Foundation – Grant/Research Support.
Mohannad Abou Saleh indicated no relevant financial relationships.
Patricia Ajayi-Fox indicated no relevant financial relationships.
Sarah Khan, MD1, Motasem Alkhayyat, MD2, Almaza A. Albakri, MD3, Sebouh Setrakian, MD2, Katherine Falloon, MD1, Mohannad Abou Saleh, MD2, Patricia Ajayi-Fox, MD2. D0333 - Gastrointestinal Hemorrhage With Gastritis and Pancolitis as Sole Presentation for Granulomatosis With Polyangiitis Flare, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
