Back

Poster Session A - Sunday Afternoon
Category: GI Bleeding
A0307 - Huge Pain in the Behind: Radiation-Induced Perforation and Bleeding Treated with Hemostatic Spray
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- SW
Scott Weismiller, DO, MS
Penn State College of Medicine
Hershey, PA
Presenting Author(s)
Scott Weismiller, DO, MS, Ronaldo Panganiban, MD, PhD, Alison Faust, MD, John Levenick, MD
Penn State College of Medicine, Hershey, PA
Introduction: Prostate brachytherapy with radiation is an effective treatment for localized prostate cancer. While generally well tolerated, radiation-associated proctopathy with resultant lower gastrointestinal (GI) bleeding is a common complication of this treatment. Rarely, prostate brachytherapy can result in rectoprostatic fistulae. There is no standard endoscopic treatment for lower GI bleeding from this complication. Increasingly, hemostatic powders are used as a “bail-out” or temporizing measure to control bleeding when the source is not amenable to other endoscopic interventions. Herein we report a case of successful control of lower GI bleeding from a rectoprostatic fistula using hemostatic spray.
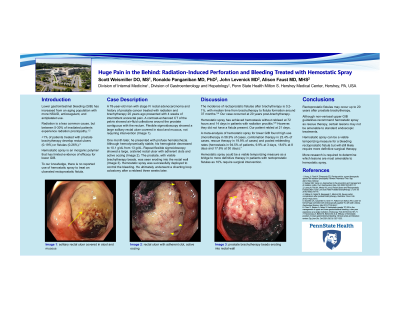
Case Description/Methods: A 78-year-old man with stage IV rectal adenocarcinoma and history of prostate cancer treated with radiation and brachytherapy 20 years ago presented with 4 weeks of intermittent anorectal pain. A contrast-enhanced CT of the pelvis showed air-fluid collections around the prostate contiguous with the rectum. Flexible sigmoidoscopy showed a large solitary rectal ulcer covered in stool and mucous, not requiring any intervention.
One month later, he presented with profuse hematochezia. Although he was hemodynamically stable, his hemoglobin decreased to 10.1 g/dL from 13 g/dL. Repeat flexible sigmoidoscopy showed a large, cratered rectal ulcer with adherent clots and active oozing. The prostate, with visible brachytherapy beads, was seen eroding into the rectal wall. Hemostatic spray was successfully deployed to control the bleeding. He ultimately underwent a diverting loop colostomy.
Discussion: The incidence of rectoprostatic fistula after brachytherapy is 0.26-1%. Fistula formation tends to occur within 37 months. Our case is rare in that rectoprostatic fistula after brachytherapy has only once been reported after 37 months, with that case being at 12 years and ours at 20 years.
To our knowledge, hemostatic spray has not been used to treat lower GI bleeding from rectoprostatic fistulae. Our experience demonstrates that this could be a viable temporizing measure in this situation. Definitive therapy may involve hyperbaric oxygen, where one patient with rectal perforation from radiotherapy was cured after 5 weeks of 24 sessions. Other considerations may be a diverting colostomy, which occurred in this patient, or proctectomy for more severe cases.
Disclosures:
Scott Weismiller, DO, MS, Ronaldo Panganiban, MD, PhD, Alison Faust, MD, John Levenick, MD. A0307 - Huge Pain in the Behind: Radiation-Induced Perforation and Bleeding Treated with Hemostatic Spray, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Penn State College of Medicine, Hershey, PA
Introduction: Prostate brachytherapy with radiation is an effective treatment for localized prostate cancer. While generally well tolerated, radiation-associated proctopathy with resultant lower gastrointestinal (GI) bleeding is a common complication of this treatment. Rarely, prostate brachytherapy can result in rectoprostatic fistulae. There is no standard endoscopic treatment for lower GI bleeding from this complication. Increasingly, hemostatic powders are used as a “bail-out” or temporizing measure to control bleeding when the source is not amenable to other endoscopic interventions. Herein we report a case of successful control of lower GI bleeding from a rectoprostatic fistula using hemostatic spray.
Case Description/Methods: A 78-year-old man with stage IV rectal adenocarcinoma and history of prostate cancer treated with radiation and brachytherapy 20 years ago presented with 4 weeks of intermittent anorectal pain. A contrast-enhanced CT of the pelvis showed air-fluid collections around the prostate contiguous with the rectum. Flexible sigmoidoscopy showed a large solitary rectal ulcer covered in stool and mucous, not requiring any intervention.
One month later, he presented with profuse hematochezia. Although he was hemodynamically stable, his hemoglobin decreased to 10.1 g/dL from 13 g/dL. Repeat flexible sigmoidoscopy showed a large, cratered rectal ulcer with adherent clots and active oozing. The prostate, with visible brachytherapy beads, was seen eroding into the rectal wall. Hemostatic spray was successfully deployed to control the bleeding. He ultimately underwent a diverting loop colostomy.
Discussion: The incidence of rectoprostatic fistula after brachytherapy is 0.26-1%. Fistula formation tends to occur within 37 months. Our case is rare in that rectoprostatic fistula after brachytherapy has only once been reported after 37 months, with that case being at 12 years and ours at 20 years.
To our knowledge, hemostatic spray has not been used to treat lower GI bleeding from rectoprostatic fistulae. Our experience demonstrates that this could be a viable temporizing measure in this situation. Definitive therapy may involve hyperbaric oxygen, where one patient with rectal perforation from radiotherapy was cured after 5 weeks of 24 sessions. Other considerations may be a diverting colostomy, which occurred in this patient, or proctectomy for more severe cases.
Disclosures:
Scott Weismiller indicated no relevant financial relationships.
Ronaldo Panganiban indicated no relevant financial relationships.
Alison Faust indicated no relevant financial relationships.
John Levenick indicated no relevant financial relationships.
Scott Weismiller, DO, MS, Ronaldo Panganiban, MD, PhD, Alison Faust, MD, John Levenick, MD. A0307 - Huge Pain in the Behind: Radiation-Induced Perforation and Bleeding Treated with Hemostatic Spray, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

