Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
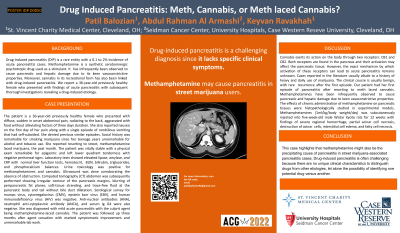
D0050 - Drug-Induced Pancreatitis: Meth, Cannabis, or Meth-Laced Cannabis?
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Patil Balozian, MD
Saint Vincent Charity Medical Center
Cleveland, OH
Presenting Author(s)
Patil Balozian, MD1, Rami Musallam, MD2, Abdul Rahman Al Armashi, MD1, Danial Nasif, MD1, Mohammad Haidous, MD1, Keyvan Ravakhah, MD2
1Saint Vincent Charity Medical Center, Cleveland, OH; 2St. Vincent Charity Medical Center, Cleveland, OH
Introduction: Drug-induced pancreatitis (DIP) is a rare entity with a 0.1 to 2% incidence of acute pancreatitis cases. Methamphetamine is a serotonergic drug used as a stimulant. It has infrequently been observed to cause pancreatic and hepatic damage due to its keen vasoconstrictive properties. Cannabis in its recreational form has also been linked with drug-induced pancreatitis. We report a 36-year-old female who presented with findings of acute pancreatitis revealing a drug-induced etiology.
Case Description/Methods: The patient is a 36-year-old previously healthy female who presented with diffuse, sudden in onset abdominal pain, radiating to the back, aggravated with food without alleviating factors of three days duration. She reported nausea on the first day of her pain along with a single episode of nonbilious vomiting that had self-subsided. Social history was remarkable for smoking marijuana since her teenage years unremarkable for alcohol and tobacco use. She reported resorting to street, methamphetamine laced marijuana, the past month. The patient was vitally stable with a physical exam remarkable for epigastric and left lower quadrant tenderness with negative peritoneal signs. Laboratory tests showed elevated lipase, amylase, and CRP with normal liver function tests, hematocrit, BUN, bilirubin, triglycerides, and phosphocalcium balances. Ultrasound was done corroborating the absence of obstruction. Computed tomography (CT) abdomen was subsequently performed showing irregular contour of the pancreatic margins, blurring of peripancreatic fat planes, soft-tissue stranding, and trace-free fluid at the pancreatic body and tail without bile duct dilatation. Serological survey for mumps virus, cytomegalovirus (CMV), epstein barr virus (EBV), and human immunodeficiency virus (HIV) was negative. Anti-nuclear antibodies (ANA), neutrophil anti-cytoplasmic antibody (ANCA), and serum Ig G4 were also negative. She was diagnosed with mild acute pancreatitis with the culprit agent being methamphetamine-laced cannabis. The patient was followed up three months after agent cessation with marked symptomatic improvement and unremarkable lab work.
Discussion: This case highlights that methamphetamine might also be the precipitating cause of pancreatitis in street marijuana-associated pancreatitis cases. Drug-induced pancreatitis is often challenging because there are no unique clinical characteristics to distinguish drugs from other etiologies, let alone the possibility of identifying one potential drug versus another.
Disclosures:
Patil Balozian, MD1, Rami Musallam, MD2, Abdul Rahman Al Armashi, MD1, Danial Nasif, MD1, Mohammad Haidous, MD1, Keyvan Ravakhah, MD2. D0050 - Drug-Induced Pancreatitis: Meth, Cannabis, or Meth-Laced Cannabis?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Saint Vincent Charity Medical Center, Cleveland, OH; 2St. Vincent Charity Medical Center, Cleveland, OH
Introduction: Drug-induced pancreatitis (DIP) is a rare entity with a 0.1 to 2% incidence of acute pancreatitis cases. Methamphetamine is a serotonergic drug used as a stimulant. It has infrequently been observed to cause pancreatic and hepatic damage due to its keen vasoconstrictive properties. Cannabis in its recreational form has also been linked with drug-induced pancreatitis. We report a 36-year-old female who presented with findings of acute pancreatitis revealing a drug-induced etiology.
Case Description/Methods: The patient is a 36-year-old previously healthy female who presented with diffuse, sudden in onset abdominal pain, radiating to the back, aggravated with food without alleviating factors of three days duration. She reported nausea on the first day of her pain along with a single episode of nonbilious vomiting that had self-subsided. Social history was remarkable for smoking marijuana since her teenage years unremarkable for alcohol and tobacco use. She reported resorting to street, methamphetamine laced marijuana, the past month. The patient was vitally stable with a physical exam remarkable for epigastric and left lower quadrant tenderness with negative peritoneal signs. Laboratory tests showed elevated lipase, amylase, and CRP with normal liver function tests, hematocrit, BUN, bilirubin, triglycerides, and phosphocalcium balances. Ultrasound was done corroborating the absence of obstruction. Computed tomography (CT) abdomen was subsequently performed showing irregular contour of the pancreatic margins, blurring of peripancreatic fat planes, soft-tissue stranding, and trace-free fluid at the pancreatic body and tail without bile duct dilatation. Serological survey for mumps virus, cytomegalovirus (CMV), epstein barr virus (EBV), and human immunodeficiency virus (HIV) was negative. Anti-nuclear antibodies (ANA), neutrophil anti-cytoplasmic antibody (ANCA), and serum Ig G4 were also negative. She was diagnosed with mild acute pancreatitis with the culprit agent being methamphetamine-laced cannabis. The patient was followed up three months after agent cessation with marked symptomatic improvement and unremarkable lab work.
Discussion: This case highlights that methamphetamine might also be the precipitating cause of pancreatitis in street marijuana-associated pancreatitis cases. Drug-induced pancreatitis is often challenging because there are no unique clinical characteristics to distinguish drugs from other etiologies, let alone the possibility of identifying one potential drug versus another.
Disclosures:
Patil Balozian indicated no relevant financial relationships.
Rami Musallam indicated no relevant financial relationships.
Abdul Rahman Al Armashi indicated no relevant financial relationships.
Danial Nasif indicated no relevant financial relationships.
Mohammad Haidous indicated no relevant financial relationships.
Keyvan Ravakhah indicated no relevant financial relationships.
Patil Balozian, MD1, Rami Musallam, MD2, Abdul Rahman Al Armashi, MD1, Danial Nasif, MD1, Mohammad Haidous, MD1, Keyvan Ravakhah, MD2. D0050 - Drug-Induced Pancreatitis: Meth, Cannabis, or Meth-Laced Cannabis?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
