Back
Poster Session D - Tuesday Morning
Category: Endoscopy Video Forum
D0187 - With a Little Help From My Friends: Percutaneously-Assisted Biliary Drain Internalization
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Jad AbiMansour, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Award: Presidential Poster Award
Jad AbiMansour, MD, Chad J. Fleming, MD, Eric J. Vargas, MD, MS, Ryan Law, DO
Mayo Clinic, Rochester, MN
Introduction: Endoscopic ultrasound (EUS)-guided hepaticogastrostomy (HG) provides endoscopic biliary drainage when conventional techniques are not feasible. Access to the biliary tree can be obtained under EUS-guided puncture of the gastric wall into the left intrahepatic ducts. In the absence of dilation, the procedure can be technically challenging.
Case Description/Methods: We present the case of a 43-year-old female with a history of total pancreatectomy for chronic pancreatitis followed by surgical revision including Roux-en-Y reconstruction and hepaticojejunostomy (HJ). The patient developed recurrent episodes of ascending cholangitis in the setting of diffuse biliary strictures and afferent limb dysmotility. She underwent placement of a percutaneous transhepatic biliary drain (PTBD) which was complicated by repeated hospitalizations for dehydration in the setting of high drain output (1-2L/day) and progressive malnutrition with marked deficiency in fat soluble vitamins. After a multidisciplinary discussion, it was felt that internalizing drainage would address these issues by promoting physiologic flow of bile.
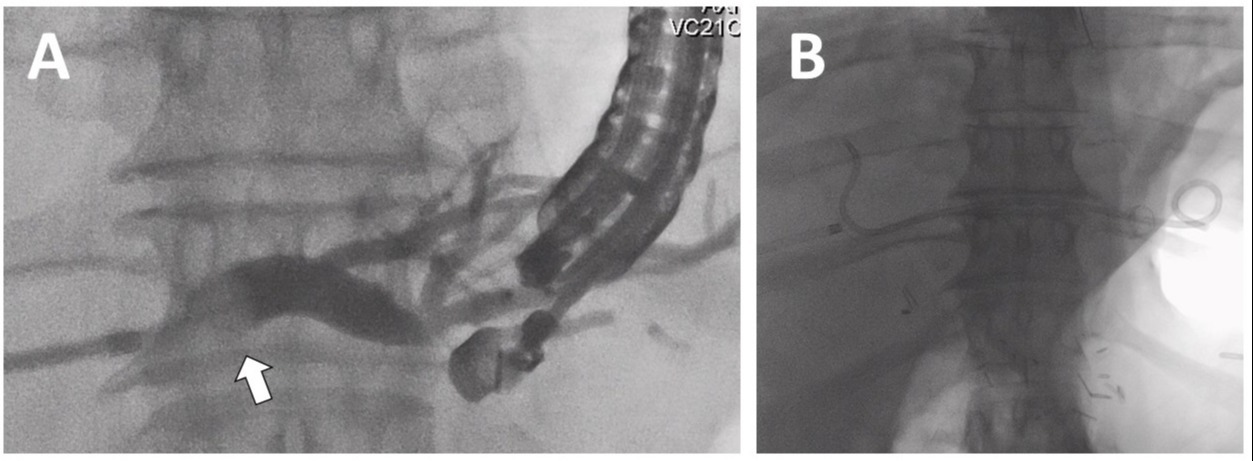
An EUS-guided HG was performed using the existing percutaneous drain tract to aid in identification and access of the left biliary tree (Video). The biliary drain was exchanged over a wire to a sheath with balloon catheter. Under fluoroscopic guidance, the percutaneous balloon catheter was advanced into the left hepatic duct and an occlusion cholangiogram was performed to opacify and distend the target ducts. The left hepatic duct was punctured under EUS-guidance with a 19-gauge needle. A 0.025” angled guidewire was then advanced into the left hepatic duct and across the HJ. After dilating the tract with a 4mm balloon, a 10mm x 8cm fully-covered self-expandable metal stent was deployed with the distal end in the left hepatic duct and proximal in the stomach. A guidewire was then used to access the right hepatic duct and a plastic double-pigtail catheter was deployed across the HG. The patient did well post-procedurally with no additional hospitalizations for cholangitis and improvement in nutrition parameters.
Discussion: Visualization of the intrahepatic ducts is critical for successful completion of EUS-HG. Here we report a creative, collaborative approach to the procedure which unencumbered the patient from external hardware and improved her nutrition through more physiologic bile circulation.
Disclosures:
Jad AbiMansour, MD, Chad J. Fleming, MD, Eric J. Vargas, MD, MS, Ryan Law, DO. D0187 - With a Little Help From My Friends: Percutaneously-Assisted Biliary Drain Internalization, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Jad AbiMansour, MD, Chad J. Fleming, MD, Eric J. Vargas, MD, MS, Ryan Law, DO
Mayo Clinic, Rochester, MN
Introduction: Endoscopic ultrasound (EUS)-guided hepaticogastrostomy (HG) provides endoscopic biliary drainage when conventional techniques are not feasible. Access to the biliary tree can be obtained under EUS-guided puncture of the gastric wall into the left intrahepatic ducts. In the absence of dilation, the procedure can be technically challenging.
Case Description/Methods: We present the case of a 43-year-old female with a history of total pancreatectomy for chronic pancreatitis followed by surgical revision including Roux-en-Y reconstruction and hepaticojejunostomy (HJ). The patient developed recurrent episodes of ascending cholangitis in the setting of diffuse biliary strictures and afferent limb dysmotility. She underwent placement of a percutaneous transhepatic biliary drain (PTBD) which was complicated by repeated hospitalizations for dehydration in the setting of high drain output (1-2L/day) and progressive malnutrition with marked deficiency in fat soluble vitamins. After a multidisciplinary discussion, it was felt that internalizing drainage would address these issues by promoting physiologic flow of bile.
An EUS-guided HG was performed using the existing percutaneous drain tract to aid in identification and access of the left biliary tree (Video). The biliary drain was exchanged over a wire to a sheath with balloon catheter. Under fluoroscopic guidance, the percutaneous balloon catheter was advanced into the left hepatic duct and an occlusion cholangiogram was performed to opacify and distend the target ducts. The left hepatic duct was punctured under EUS-guidance with a 19-gauge needle. A 0.025” angled guidewire was then advanced into the left hepatic duct and across the HJ. After dilating the tract with a 4mm balloon, a 10mm x 8cm fully-covered self-expandable metal stent was deployed with the distal end in the left hepatic duct and proximal in the stomach. A guidewire was then used to access the right hepatic duct and a plastic double-pigtail catheter was deployed across the HG. The patient did well post-procedurally with no additional hospitalizations for cholangitis and improvement in nutrition parameters.
Discussion: Visualization of the intrahepatic ducts is critical for successful completion of EUS-HG. Here we report a creative, collaborative approach to the procedure which unencumbered the patient from external hardware and improved her nutrition through more physiologic bile circulation.
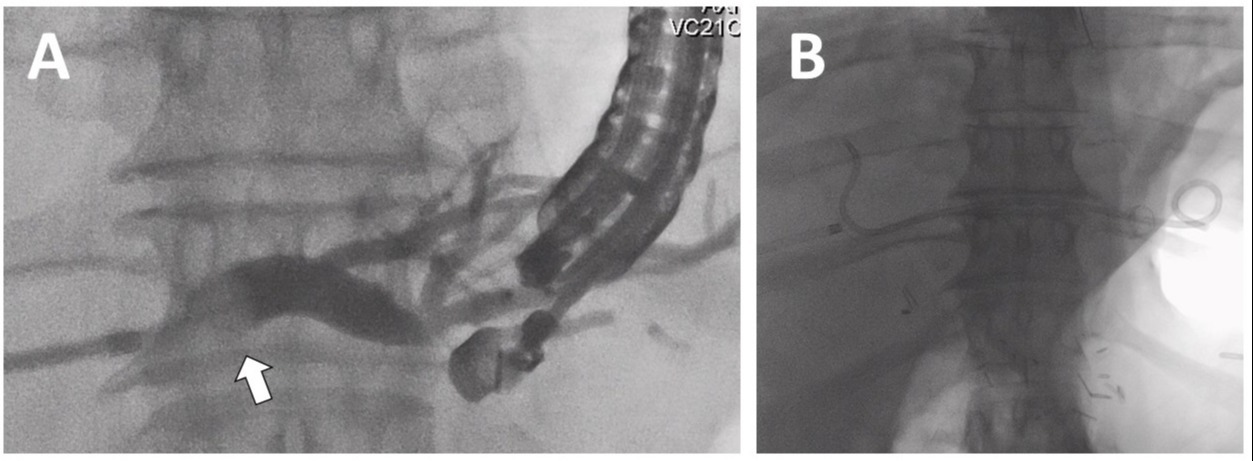
Figure: Figure 1. (A) Balloon-occlusion (arrow) cholangiogram of left hepatic duct performed through transcutaneous catheter and (B) completion fluoroscopy showing fully-covered self-expandable metal stent bridging hepaticogastrostomy with plastic stent draining the right biliary tree.
Disclosures:
Jad AbiMansour indicated no relevant financial relationships.
Chad Fleming indicated no relevant financial relationships.
Eric Vargas indicated no relevant financial relationships.
Ryan Law: Boston Scientific – Consultant. ConMed – Consultant. Medtronic – Consultant. Olympus – Consultant. UpToDate – Royalties.
Jad AbiMansour, MD, Chad J. Fleming, MD, Eric J. Vargas, MD, MS, Ryan Law, DO. D0187 - With a Little Help From My Friends: Percutaneously-Assisted Biliary Drain Internalization, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

