Back

Poster Session D - Tuesday Morning
Category: Interventional Endoscopy
D0431 - Comparison of Endoscopic Mucosal Resection versus Endoscopic Submucosal Dissection for Treatment of Rectal Neuroendocrine Tumors: A Systematic Review and Meta-Analysis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Pierce L. Claassen, BS
Washington State University Elson S. Floyd College of Medicine
Clarkston, WA
Presenting Author(s)
Connor J. Eggleston, BS1, Pierce L. Claassen, BS2, Rajani Rangray, MBBS1
1Creighton University School of Medicine, Omaha, NE; 2Washington State University Elson S. Floyd College of Medicine, Clarkston, WA
Introduction: Rectal neuroendocrine tumors (NETs) represent a small portion of gastrointestinal malignancies. Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are two treatment options of interest to therapeutic gastroenterologists. Recently the usage of EMR and ESD has increased, yet studies comparing the techniques across diverse patient populations are lacking. The aim of this systematic review and meta-analysis is to analyze the findings of all studies which compare these two treatment modalities for the management of rectal NETs.
Methods: Studies were identified by searching PubMed, Google Scholar, and reviewing citations within previously published meta-analyses. Only articles in English were included and 26 studies were selected for final analysis. The Newcastle-Ottawa Scale (NOS) was used to evaluate individual study quality. When comparing EMR to ESD, mean differences were estimated for procedure time, whereas risk ratios were calculated for histologic resection, perforation, and delayed bleeding rates (a continuity correction of 0.2 was used when any group had no adverse events). Pooled effects were estimated using random-effects meta-analysis, while between-study heterogeneity was calculated using the Paule-Mandel estimator with Hartung-Knapp adjusted standard errors. Funnel plots were used to assess publication bias.
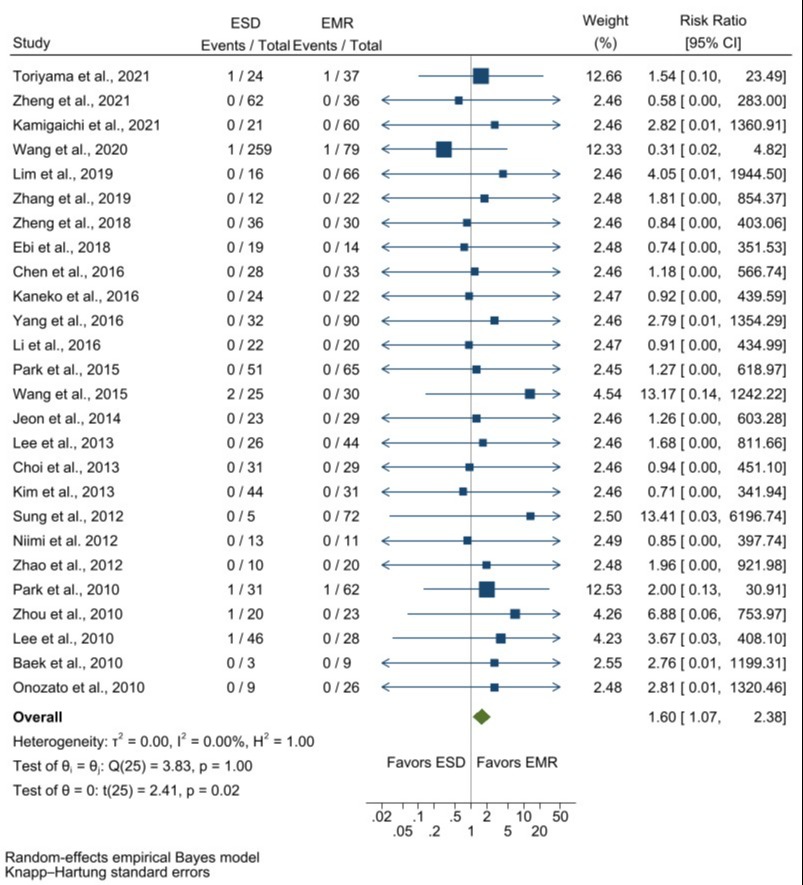
Results: Of the 26 studies, 24 were retrospective, 1 was prospective, and 1 was mixed prospective/retrospective. A total of 1,880 lesions were included from 1,863 patients. Most studies were single-center retrospective analyses and scored low on the NOS scale indicating poor methodological quality. Mean procedure time was 12.14 minutes shorter for EMR than ESD [9.99-14.30, 95% confidence interval]. Relative risk of perforation and bleeding was 1.60 [1.07-2.38] and 1.67 [1.14-2.43] times more likely, respectively when using ESD. Attaining complete histologic resection was 1.10 [1.02-1.19] times more likely with ESD.
Discussion: EMR and ESD are increasingly prevalent treatment options for superficial rectal neoplasms. Data indicates that EMR variations were superior to ESD for decreasing procedure time and minimizing perforation and bleeding rates. However, complete histologic resection was more likely with ESD. Given the poor methodologic quality of current studies, additional randomized, prospective, multicenter trials should be performed to better understand the efficacy and safety outcomes of ESD and EMR techniques for treatment of rectal NETs.
Disclosures:
Connor J. Eggleston, BS1, Pierce L. Claassen, BS2, Rajani Rangray, MBBS1. D0431 - Comparison of Endoscopic Mucosal Resection versus Endoscopic Submucosal Dissection for Treatment of Rectal Neuroendocrine Tumors: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Creighton University School of Medicine, Omaha, NE; 2Washington State University Elson S. Floyd College of Medicine, Clarkston, WA
Introduction: Rectal neuroendocrine tumors (NETs) represent a small portion of gastrointestinal malignancies. Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are two treatment options of interest to therapeutic gastroenterologists. Recently the usage of EMR and ESD has increased, yet studies comparing the techniques across diverse patient populations are lacking. The aim of this systematic review and meta-analysis is to analyze the findings of all studies which compare these two treatment modalities for the management of rectal NETs.
Methods: Studies were identified by searching PubMed, Google Scholar, and reviewing citations within previously published meta-analyses. Only articles in English were included and 26 studies were selected for final analysis. The Newcastle-Ottawa Scale (NOS) was used to evaluate individual study quality. When comparing EMR to ESD, mean differences were estimated for procedure time, whereas risk ratios were calculated for histologic resection, perforation, and delayed bleeding rates (a continuity correction of 0.2 was used when any group had no adverse events). Pooled effects were estimated using random-effects meta-analysis, while between-study heterogeneity was calculated using the Paule-Mandel estimator with Hartung-Knapp adjusted standard errors. Funnel plots were used to assess publication bias.
Results: Of the 26 studies, 24 were retrospective, 1 was prospective, and 1 was mixed prospective/retrospective. A total of 1,880 lesions were included from 1,863 patients. Most studies were single-center retrospective analyses and scored low on the NOS scale indicating poor methodological quality. Mean procedure time was 12.14 minutes shorter for EMR than ESD [9.99-14.30, 95% confidence interval]. Relative risk of perforation and bleeding was 1.60 [1.07-2.38] and 1.67 [1.14-2.43] times more likely, respectively when using ESD. Attaining complete histologic resection was 1.10 [1.02-1.19] times more likely with ESD.
Discussion: EMR and ESD are increasingly prevalent treatment options for superficial rectal neoplasms. Data indicates that EMR variations were superior to ESD for decreasing procedure time and minimizing perforation and bleeding rates. However, complete histologic resection was more likely with ESD. Given the poor methodologic quality of current studies, additional randomized, prospective, multicenter trials should be performed to better understand the efficacy and safety outcomes of ESD and EMR techniques for treatment of rectal NETs.
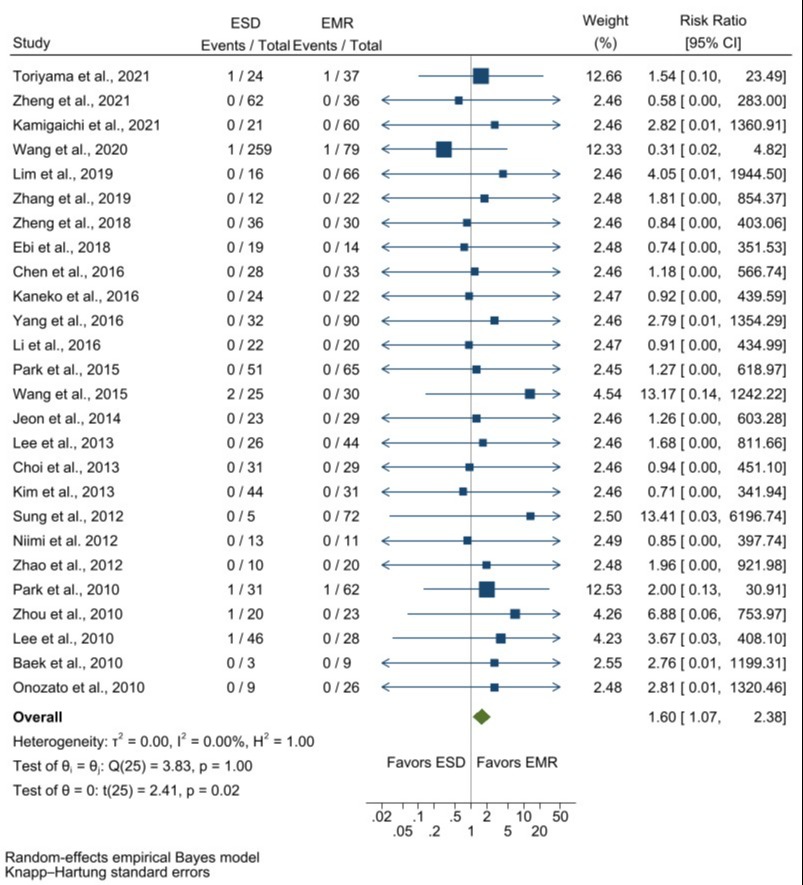
Figure: Perforation events associated with each treatment modality within individual cohort studies. When cross-comparing all studies, the overall relative risk of perforation was 1.60 [1.07-2.38, 95% confidence interval] times greater when performing endoscopic submucosal dissection (ESD) compared to endoscopic mucosal resection (EMR) for treatment of rectal neuroendocrine tumors (NETs).
Disclosures:
Connor Eggleston indicated no relevant financial relationships.
Pierce Claassen indicated no relevant financial relationships.
Rajani Rangray indicated no relevant financial relationships.
Connor J. Eggleston, BS1, Pierce L. Claassen, BS2, Rajani Rangray, MBBS1. D0431 - Comparison of Endoscopic Mucosal Resection versus Endoscopic Submucosal Dissection for Treatment of Rectal Neuroendocrine Tumors: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
