Back

Poster Session D - Tuesday Morning
Category: Interventional Endoscopy
D0432 - Safety of Endoscopic Pancreatic Necrosectomy Compared With Radiologic or Surgical Necrosectomy: A Nationwide Inpatient Analysis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Daryl Ramai, MD, MSc
University of Utah
Salt Lake City, UT
Presenting Author(s)
Award: Outstanding Research Award in the Interventional Endoscopy Category (Trainee)
Award: Presidential Poster Award
Daryl Ramai, MD, MSc1, Joseph Heaton, MD2, Dan McEntire, MD3, Saurabh Chandan, MD4, Banreet S. Dhindsa, MD5, Amaninder Dhaliwal, MD6, Douglas G. Adler, MD, FACG7
1University of Utah, Salt Lake City, UT; 2The Brooklyn Hospital Center, Brooklyn, NY; 3University of Utah Health, Salt Lake City, UT; 4CHI Health Creighton School of Medicine, Omaha, NE; 5University of Nebraska Medical Center, Omaha, NE; 6McLeod Digestive Health Center, Florence, SC; 7Centura Health-Porter Adventist Hospital, Salt Lake City, UT
Introduction: Pancreatic necrosis is an independent predictor of morbidity and mortality among patients with acute pancreatitis. Patients with pancreatic necrosis often undergo direct endoscopic necrosectomy, surgical and interventional radiology approaches exist. We compared the safety and outcomes of 3 techniques including endoscopic necrosectomy, fluoroscopy-guided necrosectomy by an interventional radiologist (IR-necrosectomy), and open necrosectomy performed by a surgeon (surgical necrosectomy).
Methods: Using the Nationwide Readmissions Database, we identified hospitalised patients who underwent pancreatic necrosectomy from 2016 to 2019. They were identified using the International Classification of Diseases, 10th Revision, Procedure Coding System. Categorical variables were described using proportions and compared with Chi-Squared Test. Continuous variables were presented as means and compared using the adjusted Wald test. Adjusted odds ratios for adverse events associated with each technique were calculated using multivariable logistic regression analysis. Adjusted hazard ratios were calculated to compare mortality rates.
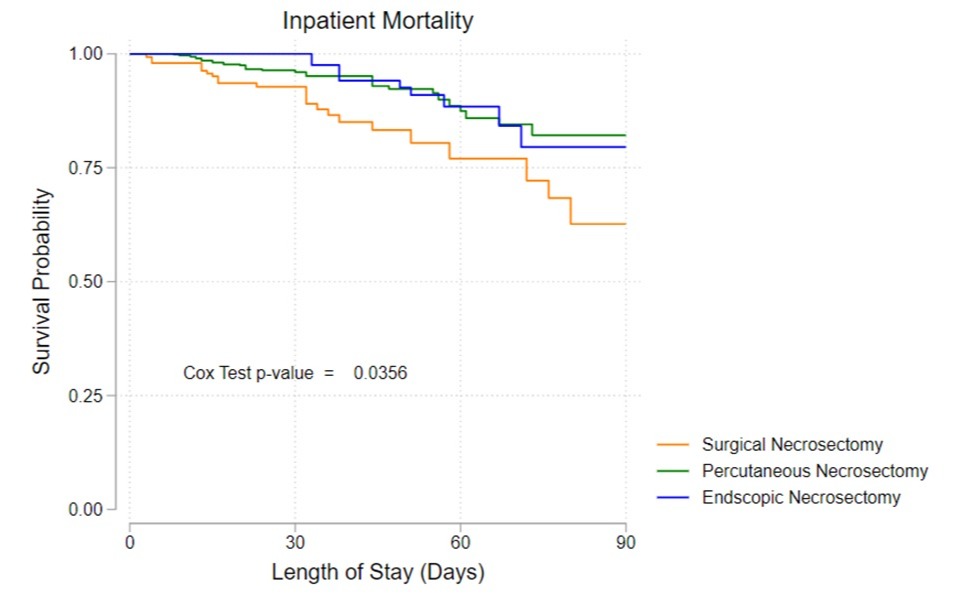
Results: Of the 2,281 patients meeting the selection criteria, the method of pancreatic necrosectomy was as follows: endoscopy, 672 (52.1 ± 1.00 years); IR, 1,338 (53.2 ± 0.56 years); and open surgery, 271 (52.0 ± 1.36 years). The rate of mortality was lowest for endoscopy (hazard ratio (HR) 0.27; 95% CI 0.08-0.90; P = 0.033) followed by IR (HR 0.44; 95% CI, 0.20-0.98; P =0.045), compared to surgery. Endoscopy was associated with less post procedure bleeding compared to IR and surgical necrosectomy, respectively (n=74 vs n=195 vs n=102; P< 0.001); as well as lower rates of post procedure end organ damage including renal failure (n=134, vs n=449, vs n= 133; P< 0.001) and respiratory failure (n=0, vs n=18, vs n= 13; P=0.002). Endoscopy was associated with average shorter lengths of stay and total hospital costs when compared with IR and surgery, respectively (20.1 vs 25.8 vs 38.3 days; P < 0.001) and ($57K vs $76K vs $123K; P< 0.001).
Discussion: Endoscopic necrosectomy is associated with significantly lower risk of inpatient mortality, adverse events, length of stay, and cost when compared to IR and surgical approaches
Disclosures:
Daryl Ramai, MD, MSc1, Joseph Heaton, MD2, Dan McEntire, MD3, Saurabh Chandan, MD4, Banreet S. Dhindsa, MD5, Amaninder Dhaliwal, MD6, Douglas G. Adler, MD, FACG7. D0432 - Safety of Endoscopic Pancreatic Necrosectomy Compared With Radiologic or Surgical Necrosectomy: A Nationwide Inpatient Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Award: Presidential Poster Award
Daryl Ramai, MD, MSc1, Joseph Heaton, MD2, Dan McEntire, MD3, Saurabh Chandan, MD4, Banreet S. Dhindsa, MD5, Amaninder Dhaliwal, MD6, Douglas G. Adler, MD, FACG7
1University of Utah, Salt Lake City, UT; 2The Brooklyn Hospital Center, Brooklyn, NY; 3University of Utah Health, Salt Lake City, UT; 4CHI Health Creighton School of Medicine, Omaha, NE; 5University of Nebraska Medical Center, Omaha, NE; 6McLeod Digestive Health Center, Florence, SC; 7Centura Health-Porter Adventist Hospital, Salt Lake City, UT
Introduction: Pancreatic necrosis is an independent predictor of morbidity and mortality among patients with acute pancreatitis. Patients with pancreatic necrosis often undergo direct endoscopic necrosectomy, surgical and interventional radiology approaches exist. We compared the safety and outcomes of 3 techniques including endoscopic necrosectomy, fluoroscopy-guided necrosectomy by an interventional radiologist (IR-necrosectomy), and open necrosectomy performed by a surgeon (surgical necrosectomy).
Methods: Using the Nationwide Readmissions Database, we identified hospitalised patients who underwent pancreatic necrosectomy from 2016 to 2019. They were identified using the International Classification of Diseases, 10th Revision, Procedure Coding System. Categorical variables were described using proportions and compared with Chi-Squared Test. Continuous variables were presented as means and compared using the adjusted Wald test. Adjusted odds ratios for adverse events associated with each technique were calculated using multivariable logistic regression analysis. Adjusted hazard ratios were calculated to compare mortality rates.
Results: Of the 2,281 patients meeting the selection criteria, the method of pancreatic necrosectomy was as follows: endoscopy, 672 (52.1 ± 1.00 years); IR, 1,338 (53.2 ± 0.56 years); and open surgery, 271 (52.0 ± 1.36 years). The rate of mortality was lowest for endoscopy (hazard ratio (HR) 0.27; 95% CI 0.08-0.90; P = 0.033) followed by IR (HR 0.44; 95% CI, 0.20-0.98; P =0.045), compared to surgery. Endoscopy was associated with less post procedure bleeding compared to IR and surgical necrosectomy, respectively (n=74 vs n=195 vs n=102; P< 0.001); as well as lower rates of post procedure end organ damage including renal failure (n=134, vs n=449, vs n= 133; P< 0.001) and respiratory failure (n=0, vs n=18, vs n= 13; P=0.002). Endoscopy was associated with average shorter lengths of stay and total hospital costs when compared with IR and surgery, respectively (20.1 vs 25.8 vs 38.3 days; P < 0.001) and ($57K vs $76K vs $123K; P< 0.001).
Discussion: Endoscopic necrosectomy is associated with significantly lower risk of inpatient mortality, adverse events, length of stay, and cost when compared to IR and surgical approaches
Figure: Kaplan-Meier survival curve comparing endoscopic, radiologic, and surgical pancreatic necrosectomy
Disclosures:
Daryl Ramai indicated no relevant financial relationships.
Joseph Heaton indicated no relevant financial relationships.
Dan McEntire indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Amaninder Dhaliwal indicated no relevant financial relationships.
Douglas Adler: Boston Scientific – Consultant.
Daryl Ramai, MD, MSc1, Joseph Heaton, MD2, Dan McEntire, MD3, Saurabh Chandan, MD4, Banreet S. Dhindsa, MD5, Amaninder Dhaliwal, MD6, Douglas G. Adler, MD, FACG7. D0432 - Safety of Endoscopic Pancreatic Necrosectomy Compared With Radiologic or Surgical Necrosectomy: A Nationwide Inpatient Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

