Back

Poster Session D - Tuesday Morning
Category: Interventional Endoscopy
D0452 - Giant Fibrovascular Esophageal Polyp Resected by Endoscopic Submucosal Dissection
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

R. Christopher Chase, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
R. Christopher Chase, MD1, David J. DiSantis, MD1, Vivek Kumbhari, MD2, Victoria Gomez, MD1, Jana G. Hashash, MD, MSc3
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Jacksonville, Jacksonville, FL; 3Mayo Clinic Florida, Jacksonville, FL
Introduction: Esophageal lipomas are rare, accounting for 1% of all benign esophageal neoplasms. Fibrovascular polyps are a subset of esophageal lipomas that can present with dysphagia, hematemesis, melena and/or profound anemia. We describe a case of a giant esophageal fibrovascular polyp (GFVP) which was treated with endoscopic submucosal dissection (ESD).
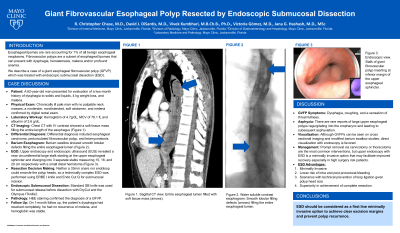
Case Description/Methods: A 62-year-old man presented for evaluation of a two-month history of dysphagia to solids and liquids, 4 kg weight loss, and melena. Examination revealed a chronically ill pale man with no palpable neck masses, a nontender, nondistended, soft abdomen, and melena confirmed by digital rectal exam. Blood work showed hemoglobin of 4.7g/dL, MCV of 78.1 fL and albumin of 3.6 g/dL. A Chest CT with IV contrast showed a soft tissue mass filling the entire length of the esophagus (Figure 1A). Differential diagnosis included esophageal carcinoma, pedunculated fibrovascular polyp, and leiomyomatosis. Barium esophagram showed smooth lobular defects filling the entire esophageal lumen (Figure 1B). Upper endoscopy and endoscopic ultrasound (EUS) revealed a near circumferential large stalk starting at the upper esophageal sphincter and diverging into 3 separate stalks measuring 15, 18, and 20 cm respectively with a small distal hematoma (Figure 1C). Because neither a 33mm snare nor endoloop could encircle the polyp heads, a technically complex ESD was performed using ERBE I knife and Endo Cut Q for submucosal incision. Standard SB knife was used for submucosal release before dissection with DryCut and the Olympus ITknife2. Hematoxylin & eosin staining confirmed the diagnosis of a GFVP. On one month follow up, the patient’s dysphagia had resolved completely, he had no recurrence of melena, and hemoglobin was stable.
Discussion: Patients with GVFPs present with dysphagia, coughing, and a sensation of throat fullness. There are rare reports of large upper esophageal polyps regurgitating into the oropharynx and leading to subsequent asphyxiation. Prompt removal via cervicotomy or thoracotomy are the most common interventions, but upper endoscopy with ESD is a minimally invasive option that may facilitate improved recovery. ESD was chosen over endoscopic mucosal resection in this case due to multiple factors: less risk of intra and post procedural bleeding, technical difficulty for loop ligation since the polyp heads were large, and for superiority of ESD at achieving complete resection.
Disclosures:
R. Christopher Chase, MD1, David J. DiSantis, MD1, Vivek Kumbhari, MD2, Victoria Gomez, MD1, Jana G. Hashash, MD, MSc3. D0452 - Giant Fibrovascular Esophageal Polyp Resected by Endoscopic Submucosal Dissection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Jacksonville, Jacksonville, FL; 3Mayo Clinic Florida, Jacksonville, FL
Introduction: Esophageal lipomas are rare, accounting for 1% of all benign esophageal neoplasms. Fibrovascular polyps are a subset of esophageal lipomas that can present with dysphagia, hematemesis, melena and/or profound anemia. We describe a case of a giant esophageal fibrovascular polyp (GFVP) which was treated with endoscopic submucosal dissection (ESD).
Case Description/Methods: A 62-year-old man presented for evaluation of a two-month history of dysphagia to solids and liquids, 4 kg weight loss, and melena. Examination revealed a chronically ill pale man with no palpable neck masses, a nontender, nondistended, soft abdomen, and melena confirmed by digital rectal exam. Blood work showed hemoglobin of 4.7g/dL, MCV of 78.1 fL and albumin of 3.6 g/dL. A Chest CT with IV contrast showed a soft tissue mass filling the entire length of the esophagus (Figure 1A). Differential diagnosis included esophageal carcinoma, pedunculated fibrovascular polyp, and leiomyomatosis. Barium esophagram showed smooth lobular defects filling the entire esophageal lumen (Figure 1B). Upper endoscopy and endoscopic ultrasound (EUS) revealed a near circumferential large stalk starting at the upper esophageal sphincter and diverging into 3 separate stalks measuring 15, 18, and 20 cm respectively with a small distal hematoma (Figure 1C). Because neither a 33mm snare nor endoloop could encircle the polyp heads, a technically complex ESD was performed using ERBE I knife and Endo Cut Q for submucosal incision. Standard SB knife was used for submucosal release before dissection with DryCut and the Olympus ITknife2. Hematoxylin & eosin staining confirmed the diagnosis of a GFVP. On one month follow up, the patient’s dysphagia had resolved completely, he had no recurrence of melena, and hemoglobin was stable.
Discussion: Patients with GVFPs present with dysphagia, coughing, and a sensation of throat fullness. There are rare reports of large upper esophageal polyps regurgitating into the oropharynx and leading to subsequent asphyxiation. Prompt removal via cervicotomy or thoracotomy are the most common interventions, but upper endoscopy with ESD is a minimally invasive option that may facilitate improved recovery. ESD was chosen over endoscopic mucosal resection in this case due to multiple factors: less risk of intra and post procedural bleeding, technical difficulty for loop ligation since the polyp heads were large, and for superiority of ESD at achieving complete resection.
Figure: Figure 1A: Sagital CT chest reveals entire esophageal lumen filled with soft tissue mass.
Figure 1B: Water soluble esophogram showing smooth lobar filling defects throughout the esophageal lumen.
Figure 1C: Endoscopic appearance of the large stalk of the multilobulated giant fibrovascular polyp inserting at the upper esophageal sphincter.
Figure 1B: Water soluble esophogram showing smooth lobar filling defects throughout the esophageal lumen.
Figure 1C: Endoscopic appearance of the large stalk of the multilobulated giant fibrovascular polyp inserting at the upper esophageal sphincter.
Disclosures:
R. Christopher Chase indicated no relevant financial relationships.
David DiSantis indicated no relevant financial relationships.
Vivek Kumbhari indicated no relevant financial relationships.
Victoria Gomez indicated no relevant financial relationships.
Jana Hashash indicated no relevant financial relationships.
R. Christopher Chase, MD1, David J. DiSantis, MD1, Vivek Kumbhari, MD2, Victoria Gomez, MD1, Jana G. Hashash, MD, MSc3. D0452 - Giant Fibrovascular Esophageal Polyp Resected by Endoscopic Submucosal Dissection, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
