Back
Poster Session D - Tuesday Morning
Category: Interventional Endoscopy
D0467 - Sporadic Inflammatory Polyp Causing Persistent Hematochezia
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Raguraj Chandradevan, MD
Augusta University Medical College of Georgia
Grovetown, GA
Presenting Author(s)
Raguraj Chandradevan, MD1, Pooja Mude, DO2, Kenneth J. Vega, MD, FACG2, Amanda Barrett, MD3, John Erikson L. Yap, MD2
1Augusta University Medical College of Georgia, Grovetown, GA; 2Augusta University Medical College of Georiga, Augusta, GA; 3Augusta University Medical College of Georgia, Augusta, GA
Introduction: Inflammatory polyps (IPs) are a rare, benign colonic entity. It can be caused by any condition that leads to prolonged inflammation or tissue injury. We present a rare case of sporadic inflammatory polyp causing persistent hematochezia which required repeated endoscopic interventions to completely resolve symptoms.
Case Description/Methods: A 43 y/o female without significant past medical history was seen due to persistent hematochezia. She denied NSAID use, family history of colon cancer/polyps, unintentional weight loss, abdominal pain or change in bowel habits. Her physical exam was unremarkable; recent laboratory parameters revealed a hemoglobin of 12.8 g/dL, and ferritin is 18ng/dL, while on oral iron supplementation, consistent with iron deficiency. Initial colonoscopy was performed by a local gastroenterologist with a 10mm sessile transverse colon polyp found and biopsied. The polyp continued to ooze necessitating hemostasis control using a hemoclip. Pathology revealed an inflammatory pseudopolyp and the patient was referred to our institution for endoscopic management. In the interim, patient continued to have hematochezia with bowel movements. Repeat colonoscopy showed an oozing sessile polyp which was completely removed via endoscopic mucosal resection (EMR) and coagulation of capillaries using the snare tip surrounding the polyp EMR site. The site was then closed by approximating mucosa using 3 hemoclips. The patient did not experience any further bleeding following intervention.
Discussion: IPs are a well-recognized entity in patients with IBD, however it can also be associated with ischemic colitis, infectious colitis, intestinal ulcers, and mucosal anastomosis. One third of the time, IPs may develop sporadically and share morphological features of epithelial polyps, adenocarcinoma, and vascular tumors. The majority are asymptomatic but can cause bleeding. Endoscopically, polyps are lined with normal edematous or superficially ulcerated mucosa. The stalk is often fibrous and vascular but may also contain muscle fascicles. IPs are confirmed with pathologic finding of inflammatory cells, replaced granulation tissues and episodic presence of hyperplastic changes. Sporadic IPs are typically treated endoscopically via polypectomy or EMR. Some cases might need ablation for bleeding control or surgical resection. Endoscopists should keep IPs in the differential diagnosis as an etiology for hematochezia.
Disclosures:
Raguraj Chandradevan, MD1, Pooja Mude, DO2, Kenneth J. Vega, MD, FACG2, Amanda Barrett, MD3, John Erikson L. Yap, MD2. D0467 - Sporadic Inflammatory Polyp Causing Persistent Hematochezia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Augusta University Medical College of Georgia, Grovetown, GA; 2Augusta University Medical College of Georiga, Augusta, GA; 3Augusta University Medical College of Georgia, Augusta, GA
Introduction: Inflammatory polyps (IPs) are a rare, benign colonic entity. It can be caused by any condition that leads to prolonged inflammation or tissue injury. We present a rare case of sporadic inflammatory polyp causing persistent hematochezia which required repeated endoscopic interventions to completely resolve symptoms.
Case Description/Methods: A 43 y/o female without significant past medical history was seen due to persistent hematochezia. She denied NSAID use, family history of colon cancer/polyps, unintentional weight loss, abdominal pain or change in bowel habits. Her physical exam was unremarkable; recent laboratory parameters revealed a hemoglobin of 12.8 g/dL, and ferritin is 18ng/dL, while on oral iron supplementation, consistent with iron deficiency. Initial colonoscopy was performed by a local gastroenterologist with a 10mm sessile transverse colon polyp found and biopsied. The polyp continued to ooze necessitating hemostasis control using a hemoclip. Pathology revealed an inflammatory pseudopolyp and the patient was referred to our institution for endoscopic management. In the interim, patient continued to have hematochezia with bowel movements. Repeat colonoscopy showed an oozing sessile polyp which was completely removed via endoscopic mucosal resection (EMR) and coagulation of capillaries using the snare tip surrounding the polyp EMR site. The site was then closed by approximating mucosa using 3 hemoclips. The patient did not experience any further bleeding following intervention.
Discussion: IPs are a well-recognized entity in patients with IBD, however it can also be associated with ischemic colitis, infectious colitis, intestinal ulcers, and mucosal anastomosis. One third of the time, IPs may develop sporadically and share morphological features of epithelial polyps, adenocarcinoma, and vascular tumors. The majority are asymptomatic but can cause bleeding. Endoscopically, polyps are lined with normal edematous or superficially ulcerated mucosa. The stalk is often fibrous and vascular but may also contain muscle fascicles. IPs are confirmed with pathologic finding of inflammatory cells, replaced granulation tissues and episodic presence of hyperplastic changes. Sporadic IPs are typically treated endoscopically via polypectomy or EMR. Some cases might need ablation for bleeding control or surgical resection. Endoscopists should keep IPs in the differential diagnosis as an etiology for hematochezia.
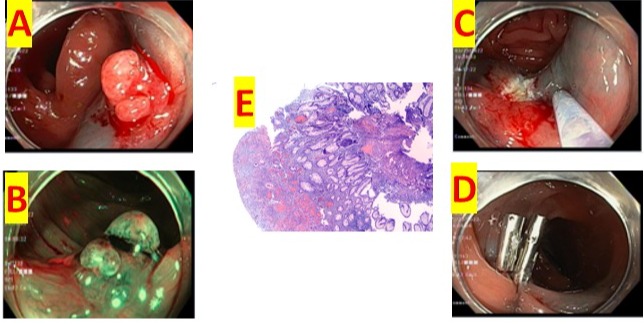
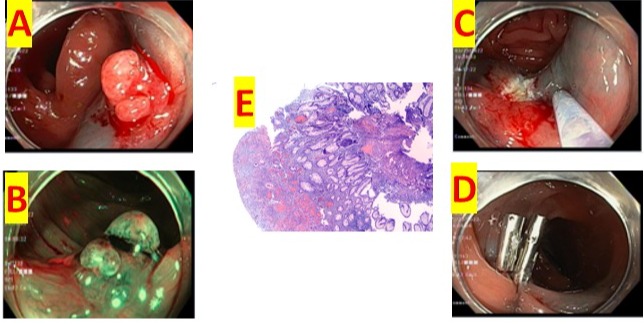
Figure: A: Magnified view of the inflammatory polyp with sessile appearance and oozing
B: Narrow band imaging view of the IP
C: Post EMR view with coagulation of the visible vessels surrounding the IP
D: Post EMR view with hemoclips deployed
E: 40x H&E: Colonic mucosa with hyperplastic changes, surfaced by a polypoid projection of granulation tissue (note prominent dilated vasculature with intervening inflammation).
B: Narrow band imaging view of the IP
C: Post EMR view with coagulation of the visible vessels surrounding the IP
D: Post EMR view with hemoclips deployed
E: 40x H&E: Colonic mucosa with hyperplastic changes, surfaced by a polypoid projection of granulation tissue (note prominent dilated vasculature with intervening inflammation).
Disclosures:
Raguraj Chandradevan indicated no relevant financial relationships.
Pooja Mude indicated no relevant financial relationships.
Kenneth Vega indicated no relevant financial relationships.
Amanda Barrett indicated no relevant financial relationships.
John Erikson Yap indicated no relevant financial relationships.
Raguraj Chandradevan, MD1, Pooja Mude, DO2, Kenneth J. Vega, MD, FACG2, Amanda Barrett, MD3, John Erikson L. Yap, MD2. D0467 - Sporadic Inflammatory Polyp Causing Persistent Hematochezia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
