Back

Poster Session D - Tuesday Morning
Category: Liver
D0500 - Understanding Barriers to Prescribing Pharmacotherapy for Alcohol Use Disorder: A Shared Responsibility
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Nicholas Noverati, MD, MEd
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Nicholas Noverati, MD, MEd, Tara Rakiewicz, MD, Kiera Chism, MD, Dina Halegoua-DeMarzio, MD, Jillian Zavodnick, MD
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Alcohol use disorder (AUD) is becoming more prevalent in the United States and has been accelerated by the global pandemic. It is essential to recognize AUD as a common precursor to the development of alcohol-related liver disease. This confers responsibility on all clinicians, especially those with specialty training in gastroenterology (GI) and hepatology, to mitigate this risk by offering any treatment that aids in abstinence. Pharmacotherapy, also known as medication-assisted treatment (MAT), for AUD is an underutilized but effective intervention that, unlike behavioral therapies, is within reach of most practicing physicians. This study aims to understand the barriers to initiating pharmacotherapy in AUD to help better inform quality improvement initiatives designed to increase the use of MAT.
Methods: A survey was conducted using the RedCap platform and sent to internal medicine (IM) hospitalists and residents, primary care physicians, and attending GI and hepatologists at one urban academic tertiary medical center. We focused on naltrexone as it is the option with the strongest evidence, lowest cost, and fewest interactions of FDA-approved MAT.
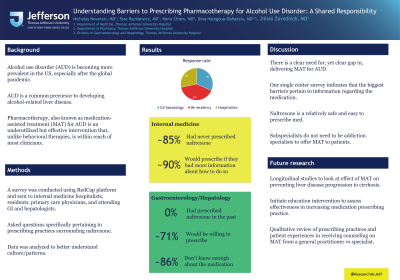
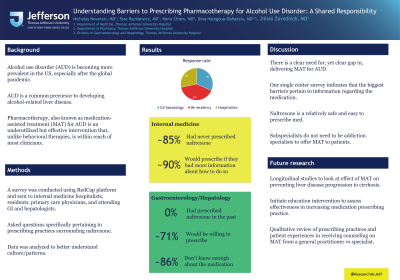
Results: The response rate was 19% (7/36) for the GI and hepatology department, 24% (29/120) for the IM residency, and 17% (5/30) for hospitalists. Within internal medicine, most (85.4%) had never prescribed naltrexone for AUD, but 89.6% would if they had more information about how to do so. The most popular barriers identified included: not knowing enough about the medication (70.8%), specifically not knowing the contraindications (56.3%), and prescribing did not occur to them (54.2%). Within GI and hepatology, 0% had prescribed naltrexone, 71.4% said they would be willing, but 85.7% said they didn’t know enough about the medication.
Discussion: Alcohol use is increasing in the US, and many patients may benefit from assistance with abstinence and reducing cravings by using FDA-approved MAT such as naltrexone. Initiating treatment in the inpatient setting may be a valuable opportunity to reach such populations. This study showed an apparent deficit among participants within IM, GI, and hepatology departments in prescribing naltrexone, primarily due to a lack of knowledge of available medications and their appropriate use. These findings will assist quality improvement initiatives at our institution aimed at increasing inpatient naltrexone initiation and may also help inform other institutions’ efforts.

Disclosures:
Nicholas Noverati, MD, MEd, Tara Rakiewicz, MD, Kiera Chism, MD, Dina Halegoua-DeMarzio, MD, Jillian Zavodnick, MD. D0500 - Understanding Barriers to Prescribing Pharmacotherapy for Alcohol Use Disorder: A Shared Responsibility, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Alcohol use disorder (AUD) is becoming more prevalent in the United States and has been accelerated by the global pandemic. It is essential to recognize AUD as a common precursor to the development of alcohol-related liver disease. This confers responsibility on all clinicians, especially those with specialty training in gastroenterology (GI) and hepatology, to mitigate this risk by offering any treatment that aids in abstinence. Pharmacotherapy, also known as medication-assisted treatment (MAT), for AUD is an underutilized but effective intervention that, unlike behavioral therapies, is within reach of most practicing physicians. This study aims to understand the barriers to initiating pharmacotherapy in AUD to help better inform quality improvement initiatives designed to increase the use of MAT.
Methods: A survey was conducted using the RedCap platform and sent to internal medicine (IM) hospitalists and residents, primary care physicians, and attending GI and hepatologists at one urban academic tertiary medical center. We focused on naltrexone as it is the option with the strongest evidence, lowest cost, and fewest interactions of FDA-approved MAT.
Results: The response rate was 19% (7/36) for the GI and hepatology department, 24% (29/120) for the IM residency, and 17% (5/30) for hospitalists. Within internal medicine, most (85.4%) had never prescribed naltrexone for AUD, but 89.6% would if they had more information about how to do so. The most popular barriers identified included: not knowing enough about the medication (70.8%), specifically not knowing the contraindications (56.3%), and prescribing did not occur to them (54.2%). Within GI and hepatology, 0% had prescribed naltrexone, 71.4% said they would be willing, but 85.7% said they didn’t know enough about the medication.
Discussion: Alcohol use is increasing in the US, and many patients may benefit from assistance with abstinence and reducing cravings by using FDA-approved MAT such as naltrexone. Initiating treatment in the inpatient setting may be a valuable opportunity to reach such populations. This study showed an apparent deficit among participants within IM, GI, and hepatology departments in prescribing naltrexone, primarily due to a lack of knowledge of available medications and their appropriate use. These findings will assist quality improvement initiatives at our institution aimed at increasing inpatient naltrexone initiation and may also help inform other institutions’ efforts.

Figure: Figure 1. Responses from gastroenterologists, hepatologists, and internal medicine residents and hospitalists, to questions regarding barriers to prescribing naltrexone. GI= gastroenterology; IM=Internal Medicine
Disclosures:
Nicholas Noverati indicated no relevant financial relationships.
Tara Rakiewicz indicated no relevant financial relationships.
Kiera Chism indicated no relevant financial relationships.
Dina Halegoua-DeMarzio indicated no relevant financial relationships.
Jillian Zavodnick indicated no relevant financial relationships.
Nicholas Noverati, MD, MEd, Tara Rakiewicz, MD, Kiera Chism, MD, Dina Halegoua-DeMarzio, MD, Jillian Zavodnick, MD. D0500 - Understanding Barriers to Prescribing Pharmacotherapy for Alcohol Use Disorder: A Shared Responsibility, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
